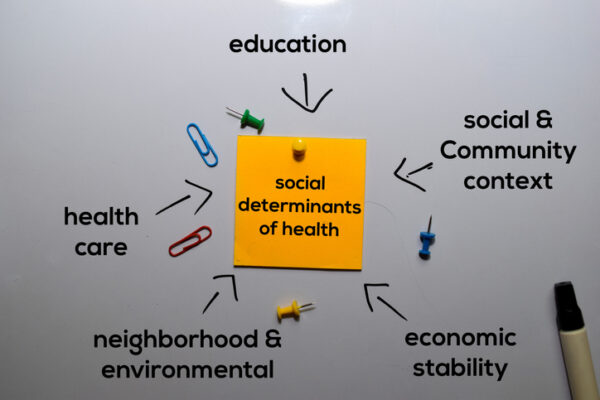
As the conversation around addressing social determinants of health gains steam, a key player has emerged: healthcare information exchanges.
HIEs that were created to further healthcare interoperability appear to be expanding their mandate to include efforts to address social determinants of health.
For instance, HIEs like CyncHealth are incorporating tools to help healthcare stakeholders more effectively tackle social determinants of health issues. That’s because they are uniquely positioned to effectively coordinate disparate efforts, said Melanie Surber, chief clinical officer of Nebraska’s statewide HIE CyncHealth, at the virtual ONC 2021 Annual Meeting Monday.
CyncHealth is rolling out a solution that aims to help providers, payers and community-based organizations coordinate care to address social determinants of health. The rollout is slated to be completed by July.
“If we do not address the social determinants of health when it comes to taking care of the individuals we serve, we are missing part of the story,” said Surber.
The HIE realized there was a need for this type of statewide solution as healthcare stakeholders were operating in silos with completely separate databases and solutions.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
CyncHealth was in a prime position to connect all the necessary entities as it already had a statewide infrastructure connected to providers, payers and many community resources. It also had a master patient index and the ability to aggregate patient records, Surber said.
The solution allows for easy data flow between the different entities. For example, if a patient is discharged from the hospital with a referral for social services, their payer and community-based organizations in the area receive a notification. These entities can then work with the patient to address their needs.
“Everything stays connected and all the communication stays in the platform,” Surber said.
Further, providers seeking social service referrals for their patients can drill down into resources based on accessibility standards, language or distance. This is especially helpful for patients in rural areas, whose access to social services may be limited, Surber said.
Like Nebraska’s CyncHealth, Ohio’s state HIE saw the need to better coordinate local efforts to address social factors that contribute to one’s health.
“In the midst of the pandemic, our board, our stakeholders, and many of the organizations that we work with felt it was important to really start to address equity, health disparities, racism,” said Dan Paoletti, CEO of the Ohio Health Information Partnership, at the ONC 2021 Annual Meeting. “They also felt we were in a unique position — because of the variety of stakeholders that were part of our board, the heart of our stakeholder group — to really try to address some of these issues.”
The HIE decided to focus on a specific care area: pregnancy, prenatal care and infant mortality. For six months, they conducted interviews with providers, payers, public health agencies and community organizations to better understand the barriers and roadblocks to care that were causing poor outcomes in this area.
“What we found is there is a significant issue with data and information gaps, not so much from a clinical interoperability perspective…but it was really around once [the patient] left the health system,” Paoletti said.
They uncovered a specific need to standardize education and support materials for pregnant women and those with infants. The Ohio Health Information Partnership brought together the necessary resources and standardized the materials so they could be understood by people with different backgrounds, Paoletti said.
The organization is also encouraging the adoption of interoperability standards to support social determinants of health data exchange. The 360x ONC project provides two IHE International-approved standards: one for closed-loop referral and another for ambulatory/acute transfer to a skilled nursing facility.
Paoletti hopes that these standards will broadly be adopted by the end of this year, which will be “transformative.”
“We feel very strongly that creating these data standards and interoperability among the social service organizations and community-based organizations is critical,” he said.
If HIEs are successful in integrating social factors with clinical care, we may be one step closer to better healthcare for all.
Photo: syahrir maulana, Getty Images













