
In an effort to reduce health inequities, two companies are joining forces to combine a trove of health plan member data with information on race, ethnicity and language.
The companies are Chicago-based Blue Health Intelligence, a licensee of the Blue Cross Blue Shield Association, and Dunwoody, Georgia-based data company AnalyticsIQ, which announced a partnership on Monday.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
They will combine Blue Health Intelligence’s database, which includes commercial health plan data from Blues members across the U.S., with AnalyticsIQ’s capabilities to draw insights that Blues plans can then use to design more equitable community partnerships and intervention programs, said Swati Abbott, CEO of Blue Health Intelligence, in an email.
Through the partnership, Blue Health Intelligence will augment its database — which includes more than 60 million current health plan members and over 200 million members in the last 12 years — with race, ethnicity and language information and numerous social determinants of health factors, Abbott said. The partnership will add 13 ethnicity-and language-related data elements to the database, including “Southeast Asian,” “Middle Eastern” and “Polynesian.”
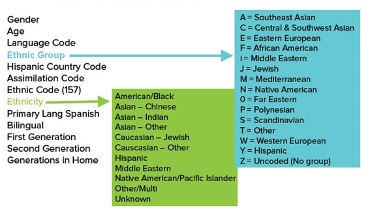
“AnalyticsIQ provides a depth and breadth of ethnic data intelligence that ranges from an individual’s core ethnic grouping and ethnic sub-group to their country of origin and primary language,” she said.
These data elements are especially useful for Blue Health Intelligence because it provides lifestyle insights that can be used to improve member experience and engagement.
For example, health plans can use the stratified data to align Spanish-speaking care managers with members whose primary language is Spanish from the time they are first enrolled in the program. This could increase a plan’s ability to both lower healthcare costs and improve outcomes, Abbott said.
“The data points provided by AnalyticsIQ are truly fundamental to who people are,” said Dave Kelly, CEO of AnalyticsIQ, in an email. “That understanding is the first step towards better outcomes.”
Increasingly, payers are focusing on tackling health inequities, spurred by a pandemic that hit people of color the hardest. In April, the Blue Cross Blue Shield Association announced its new national health equity strategy, which will focus on four conditions that disproportionately affect communities of color: maternal health, behavioral health, diabetes and cardiovascular conditions.
Photo: 9amstock, Getty Images, Blue Health Intelligence














