Novartis is stopping a mid-stage clinical trial of a drug for preventing organ rejection after an early look at data in kidney transplant patients showed the experimental treatment was less effective compared to the standard of care therapy.
The Swiss pharmaceutical giant did not disclose specific details about the interim study results for the drug, iscalimab. Novartis said Friday that it is still reviewing the data and when that review is complete, it will share the results with the broader scientific community.
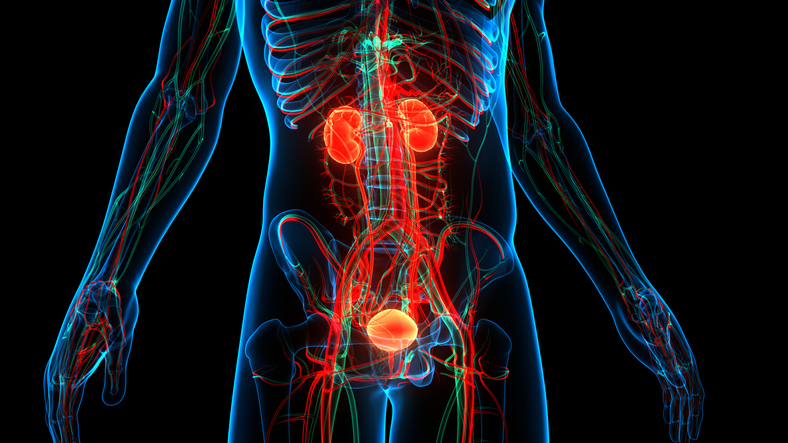
Iscalimab is a monoclonal antibody designed to target and block a receptor, CD40, that’s part of a pathway activated in organ rejection. Novartis had described iscalimab as offering the prospect of “one transplant for life.” With currently available therapies, a kidney transplant lasts about 10 years, after which the patient must return to dialysis, the company said in a 2019 investor presentation. Those patients have a poor quality of life and more than half of them die within five years. The alternative is another kidney transplant, which depletes the pool of donor organs. Iscalimab, Novartis said in the presentation, could enable a transplant to last 20 years. By avoiding the need for patients to undergo a second transplant surgery, the drug would preserve the donor organ pool for new patients, the company said.
Novartis posted encouraging results for the transplant drug in 2019, albeit, from a small patient sample. According to data presented at the American Transplant Congress, outcomes in those treated with iscalimab were better compared to those who received tacrolimus, the anti-rejection drug that is the standard of care. In three of the five patients treated with the Novartis drug, examination under a microscope found that kidney tissue was normal compared to none of the seven who were given tacrolimus.
Based on the encouraging clinical data, Novartis proceeded to a Phase 2 study enrolling 418 patients. Like the preceding study, patients were randomly assigned to receive either iscalimab or tacrolimus. In both groups, the therapies were given in combination with other steroids and other immunosuppressive treatments. The main goal was a composite, measuring the proportion of patients who rejected the organ, lost organ function, or died.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Share some of the trends you are seeing among your clients across healthcare, including chronic conditions, behavioral health, healthcare navigation, and more.
Novartis has long pitched iscalimab’s approach as having potential use in multiple immunological indications. Clinical trials in liver transplant, Sjogren’s syndrome, and hidradenitis suppurativa are ongoing.
Others are also pursuing potential therapies that could improve outcomes for organ transplant patients. Talaris Biotherapeutics is developing a cell therapy made with immune and stem cells from the person who donated the organ. The Louisville, Kentucky-based company is now in late-stage clinical trials testing its approach in kidney transplant patients. In its early days, the biotech developed its technology under an alliance with a large pharmaceutical company—Novartis.
Forte Bio’s live biotherapeutic fails to beat placebo in atopic dermatitis
Treatments available for the itchy skin and redness caused by atopic dermatitis include drugs that circulate in the body and suppress the immune system, potentially sparking a range of side effects along the way. Forte Biosciences aimed to avoid those problems with a topical product comprised of three strains of Gram-negative bacteria that the company selected to address inflammatory skin disease. The approach of the experimental treatment, FB-401, was intended to drive tissue repair and tamp down inflammation. The company also hoped the drug would suppress harmful bacteria.
In preliminary results from a Phase 2 study, Forte said that the drug failed to demonstrate statistical significance against the main goal of showing at least 50% improvement according to a scale that measures atopic dermatitis severity. The results showed that 58% of patients given the Forte drug achieved that goal, beating the 50% mark it needed to hit. But in the placebo group, 60% of participants reached the study’s main goal.
Forte CEO Paul Wagner said in a statement that the company will continue to analyze the FB-401 data, but the company will not advance development of the drug any further. An update on the company’s future plans will come “over the next several months,” he said.
Takeda cancer drug fails to show statistical significance in Phase 3
Pevonedistat, a Takeda Pharmaceutical drug being developed as a first-line treatment for certain blood cancers, failed a Phase 3 clinical trial. The small molecule drug was designed to block NEDD8-activating enzyme, an approach intended to spark cell death by disrupting protein homeostasis in cancer cells.
The Japanese pharmaceutical giant was testing pevonedistat, in combination with the chemotherapy azacitidine, as a treatment for higher-risk myelodysplastic syndromes, chronic myelomonocytic leukemia, and low-blast acute myeloid leukemia. That combination was compared to treatment with azacitidine alone. The main goal was to show improvement in event-free survival—how long the patient remains free of events or complications after the end of the primary treatment. Takeda said that the drug did not achieve statistical significance for that goal. The company added that full results will be submitted for presentation at a future medical meeting.
Image: Getty Images, magicmine














