A BridgeBio Pharma drug that the company had touted as potentially better than an approved Pfizer product at addressing the protein at the root of a rare heart disorder has instead failed to beat a placebo in the first part of a pivotal clinical trial. BridgeBio calls the results “baffling,” and executives have more questions than answers, but they’re also still holding out hope for the experimental treatment, pointing to the second part of the Phase 3 clinical trial—which is not expected to post data for another year or more.
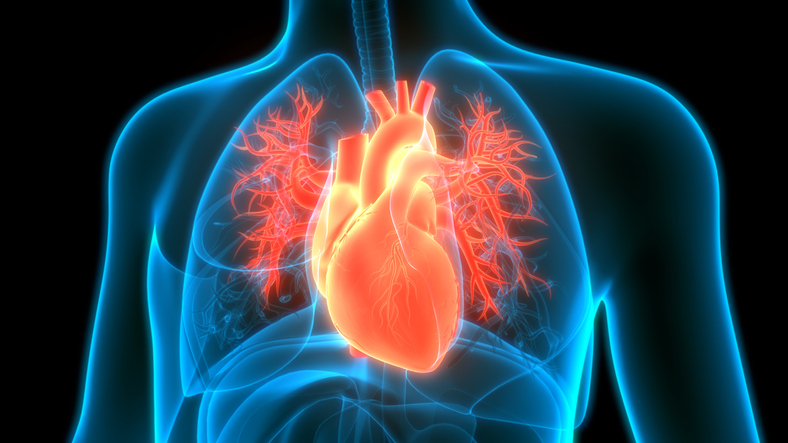
The BridgeBio drug, acoramidis, is being developed to treat transthyretin amyloidosis (ATTR), a rare and life-threatening disease that can cause a thickening of the heart muscle that impedes its function, potentially leading to heart failure. ATTR can be inherited but in people without genetic mutations the disorder can still develop as a normal part of aging.
A total of 632 participants representing both causes of ATTR were enrolled in the placebo-controlled Phase 3 clinical trial. The main goal of the first part of the study was to show, after 12 months of treatment, improvement according to a test that assessed how far patients could walk in six minutes. Performance on this test declines with age. In healthy elderly adults, the typical decline is only 7 meters in 12 months.
According to preliminary results released by Palo Alto, California-based BridgeBio on Monday, the average decline in patients treated with acoramidis was 9.28 meters—not enough to show a statistically significant difference compared to the average 7.04 meter decline in the placebo group. In an investor presentation, BridgeBio said the placebo arm in the study “substantially outperformed” historical controls, with a decline that more closely tracked with the decline typically observed in healthy elderly adults. Furthermore, the placebo group of the BridgeBio study outperformed, by more than 70%, the placebo group in the pivotal study of Pfizer’s ATTR drug, Vyndaqel, which was approved in 2019. In 2020, that drug and a second formulation named Vyndamax accounted for nearly $1.3 billion in revenue, according to Pfizer’s financial statements.
In Monday’s announcement, BridgeBio CEO Neil Kumar called the acoramidis results “disappointing and baffling.” The Phase 3 test of acoramidis enrolled patients similar to those enrolled in the pivotal study for Vyndaqel, BridgeBio noted in the investor presentation. The current hypothesis for the surprising placebo result is context bias, training bias, and an evolution in the approaches to diagnosing and treating ATTR, according to the company.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
ATTR develops when a protein called transthyretin is misfolded, resulting in a destabilized form that leads to deposits of amyloid on nerves and organs, including the heart. It’s estimated to affect more than 400,000 people worldwide, according to BridgeBio. In 2018, the FDA approved Alnylam Pharmaceuticals drug Onpattro as a treatment for the hereditary form of ATTR that affects the nerves. Onpattro uses RNA interference, “silencing” the gene that produces the protein at the root of the disorder. Later that year, the FDA approved Tegsedi, a drug developed by Akcea Therapeutics and Ionis Pharmaceuticals to treat the nerve pain caused by hereditary ATTR. That drug is an antisense oligonucleotide designed to bind to transthyretin and degrade it.
Though Pfizer’s Vyndaqel was the first drug approved to treat ATTR that affects the heart, BridgeBio’s proposition was that its drug works better. Acoramidis is a small molecule designed to bind to transthyretin and stabilize it, which in turn reduces the level of amyloid formation, potentially slowing or even halting disease progression. Pfizer’s Vyndaqel is also a small molecule transthyretin stabilizer, but BridgeBio has described its drug as better at protein stabilization. During the company’s R&D day in October, executives pointed to head-to-head lab test results showing that a lower dose of acoramidis was better than either of the doses of Pfizer’s drug, achieving “near-complete stabilization” of transthyretin.
Despite missing the main goal of the Phase 3 study, BridgeBio noted its drug showed improvements according to a questionnaire that measures quality of life, a cardiac biomarker, and a test that measures the concentration of transthyretin in the blood. The drug was also well tolerated by patients in the clinical trial with no signs of safety problems. For those reasons, the independent data monitoring committee assessing the progress of the Phase 3 clinical trial is recommending that the acoramidis study continue. The clinical trial was designed as a 30-month study, and BridgeBio said that the committee and the company agree that there is potential for acoramidis to show patient benefit at that point. In addition to further assessing changes in the six-minute walk test, the goals at month 30 include two measures: the frequency of hospitalization for cardiovascular reasons as well as deaths from all causes.
“The drug does appear to be pharmacologically active and well-tolerated, and we observed improvement on quality of life with promising trends on adverse events leading to death,” Kumar said. “The drug seems to be doing what we are asking of it. If we observe enough clinical outcome events at month 30, I am still hopeful that we will demonstrate the benefit of acoramidis treatment.”
Acoramidis was the lead product candidate of Eidos Therapeutics, a company that spun out of BridgeBio and became publicly traded in 2018, though its former parent retained a majority stake. Nearly a year ago, BridgeBio completed its acquisition of the shares of Eidos it did not own, giving it control of the ATTR program.
BridgeBio said the Phase 3 study of acoramidis is already fully funded through completion. The company’s cash reserves currently total $800 million; an additional $300 million in milestone payments could be coming if other assets in the pipeline hit key goals in the coming year. BridgeBio expects four other clinical-stage programs could post crucial data in 2022. But preliminary data from the second part of the acoramidis Phase 3 study are not expected until 2023.
The disappointing data reported on Monday battered BridgeBio’s stock price, which fell to $11.61 per share in mid-day trading, down more than 71% from the closing price last Thursday, ahead of the Christmas holiday.
Image: Magicmine, Getty Images












