
A new report finds that a slight majority of doctors and nurses globally feel that telehealth could undermine their efforts at demonstrating empathy for patients.
The conclusions come from an online 15 minute survey of 2,838 in the field spanning 111 countries conducted by New York-based Elsevier Health. 1,691 doctors and 1,108 nurses took the survey. Further, the report drew on 60-minute discovery interviews with 23 healthcare leaders as well as on three roundtable discussions with leaders in the U.K., China, and the U.S. The report explored attitudes toward technology adoption, current issues driving change, and offers predictions of what being a clinician may look like in 10 years.
Partnering with patients to manage their health
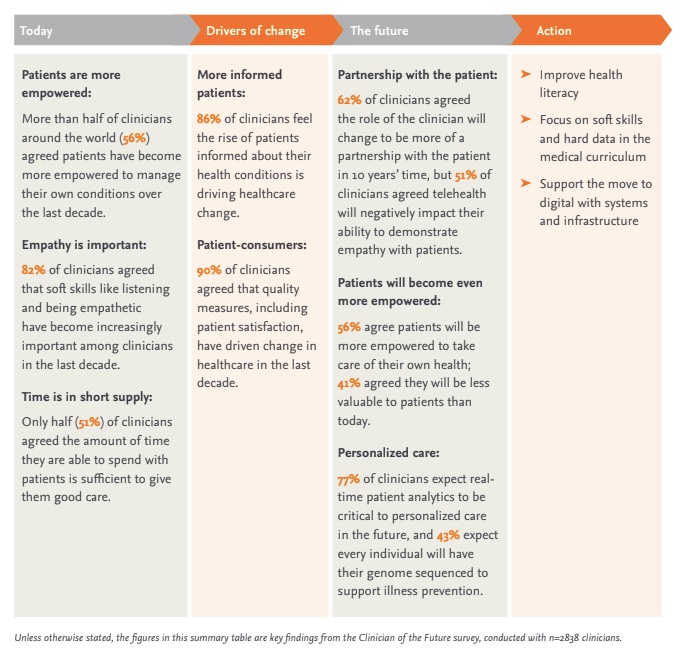
First, 56% of clinicians said they see patients as more empowered to address their health now than over the past ten years, according to the report. This figure paralleled the 62% of clinicians who said in the upcoming decade they see the patient/doctor relationship shifting into more of a partnership.
Technology increasingly plays a role in that relationship. However, over half — 51% — of clinicians felt telehealth would harm their ability to demonstrate empathy with their patients, according to the report. Despite this concern, those surveyed seemed to think technology would play an ever-increasing role in medicine. For example, 77% reported expecting real-time patient analytics to be crucial in personalized care moving forward. In a similar vein, 43% anticipated that patients will turn to genome sequencing in order to support illness prevention.
“When applied correctly, technology can streamline inefficiencies and workflows, and highlight clinical insights, while data can help clinicians deliver better care to their patients,” said Hemalee Patel, senior medical director of chronic care management and clinical design lab at One Medical who contributed to the report, in an email.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
Patel added that remote patient monitoring of blood pressure devices, continuous glucose monitors and pulse oximeters, are a few ways that clinicians can provide real time personalized care to their patients.
“This has led to improved medical adherence, and increased levels of compliance and transparency between clinician and patient,” she said. “Proper technology training is a critical aspect for all this. I agree with the 83% of clinicians in the report [who] believe that training needs to be overhauled.”
Shift to total health
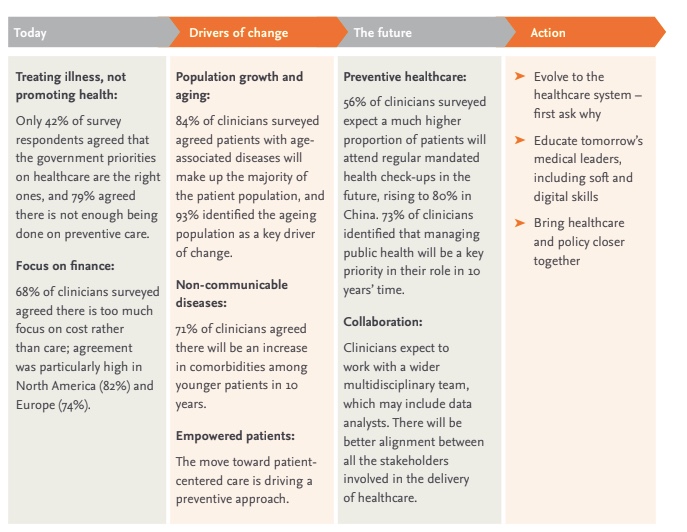
A vast majority at 79% said what is done for preventive care is not enough, the report stated. Looking to the patients they expect to treat, 71% said they anticipate a rise in noncommunicable diseases with co-morbidities for younger patient populations.
Further, in the next decade, clinicians anticipate a more preventive care approach for both mental and physical health, the report said. As a factor driving this shift, clinicians said they anticipate working in a diverse expanded team, including experts like data analysts.
Technology on the rise, again
The pandemic accelerated the use of technology for healthcare indications, and that trend is expected to continue throughout the next decade, pandemic or not, the report predicted. For example, 63% said they think most consultations will be remote in ten years time. And 56% anticipate using support tools with artificial intelligence (AI) to make most decisions.
“Although clinicians are certainly smart enough to adopt new technologies and integrate them into their skills sets, they can’t be expected to ‘build the airplane while flying it,’ while patient lives are at stake,” said Marion Broome, a professor of nursing at Duke University, School of Nursing, who contributed to the report in an email. “Therefore, engaging clinicians in training will require compensation in terms of their time and energy. The days of clinician ‘armchair training’ (i.e. reading journals, fire and safety training, etc.,) which were typically handled after a long workday are over. Instead, development and training should be considered as an essential part of the financial costs for quality care.”
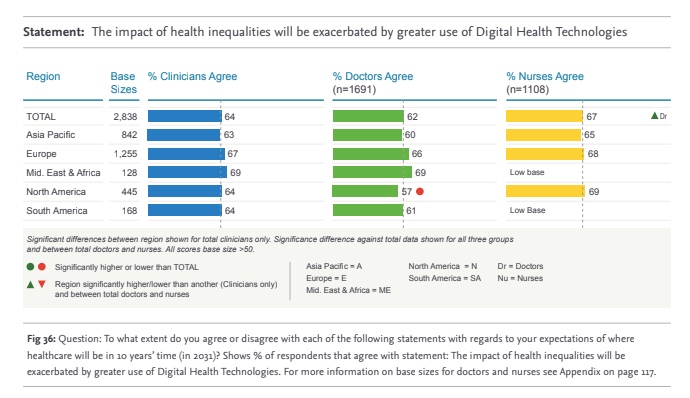
Despite the continued expected surge in digital health, 64% of clinicians expressed concern that digital technologies will exacerbate health inequities.
Clinicians balancing burnout
On average, clinicians are working 50 hours a week, according to the report. Further, just 57% of them reported having a positive work-life balance. And they think their role is taking a turn for the worse. Despite the challenge to balance it all, 85% of clinicians said they enjoy their jobs.
“In addition to deepening pre-pandemic health disparities, Covid also amplified burnout among frontline workers,” said Leo Celi, clinical research director and principal research scientist for the laboratory of computational physiology (LCP) at MIT and attending physician specialist at the Beth Israel Deaconess Medical Center in Boston who contributed to the report, in an email. “As the population ages, the proportion with chronic medical conditions is expected to grow. Unless the workforce expands to address high burnout rates and shorter tenure, more task shifting to technicians and technology will be needed. This will require clinician-directed redesign of the workflow, a task that in turn requires a skill that is not taught in pharmacy, nursing or medical school.”
This balancing act is likely to persist, with 68% of clinicians anticipating a doctor shortage in the next decade and 74% expecting one for nurses.
“Overall, clinician burnout and the healthcare workforce shortage are very serious problems that we continue to face and could get worse over time. In fact, the report found that nearly half of all U.S. doctors and nurses anticipate leaving their role in the next 2-3 years, with nearly half of this group either retiring or moving out of health care entirely,” said Jan Herzhoff, president of Elsevier Health, in an email. “It is also worth noting the other half, while staying in healthcare, is planning to switch their employer which will increase competition for talent and create disruptions for health systems.”
Given the expected shortage, Herzhoff had several recommendations to tackle it head on, such as incentivize new talent to the field. He also offered scaling educational opportunities and making sure professionals in healthcare receive continuous education to stay up to date on technology and health data best practices as crucial steps.
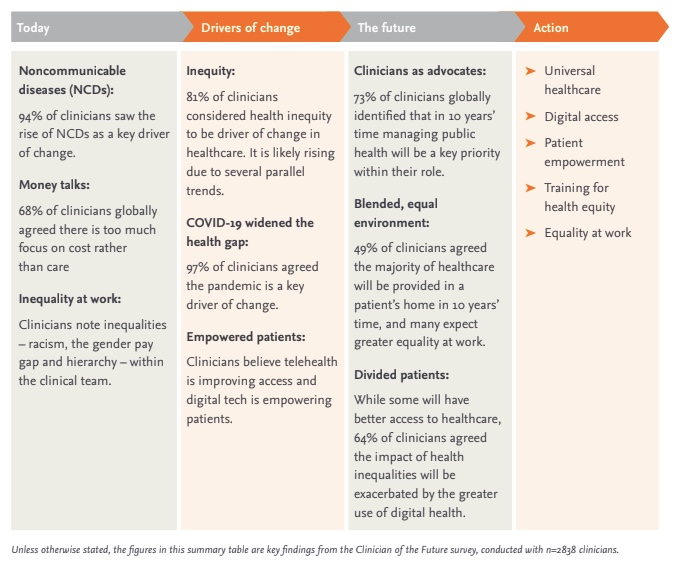
Photo: HASLOO, Getty Images; graphs/charts: Elsevier Health












