Last week, the American Association for Cancer Research released its annual report on the progress of cancer care in the U.S.
Deaths from cancer continue to decrease due to advances in research, screening and treatment, according to the report. It found that the country’s cancer death rate had fallen by 32% from 1991 to 2019 — a reduction that translates to 3.5 million lives being saved, Dr. David Cohn, interim CEO and chief medical officer at Ohio State University’s James Cancer Hospital, said in an interview.
To keep moving in the right direction and decrease cancer mortality rates even further, oncologists must prioritize personalized cancer treatment and initiatives to address social determinants of health, Dr. Cohn exhorted.
A few different factors are contributing to the country’s declining cancer death rate — the first one Dr. Cohn pointed to is the mitigation of risk factors through lifestyle changes such as smoking cessation. For example, the report showed that 42% of U.S. adults smoked cigarettes in 1965, whereas just 12.5% did in 2020. Smoking tobacco increases a person’s risk of developing not only lung cancer, but also 17 other types of cancer, including bladder, kidney and pancreatic and liver, according to the report.
Early screening is another key reason cancer death rates are falling. Over the past decade, advanced cancer detection technology has created tests that can catch the disease at its earliest stage before it has spread to multiple sites in the body. However, while many have benefited from early screening, not all can equally leverage these tests. Early screening often misses the country’s uninsured population as they visit the doctor infrequently in order to avoid expensive bills, according to the report.
Technological advancements in cancer screening are expected to continue over the coming years, as evidenced by FDA approvals of AI-powered software to aid early cancer detection and diagnosis, the report said. For example, Memorial Sloan Kettering spinout Paige received FDA clearance last year for its cancer detection tool, which is the first AI-based software approved by FDA to identify cancerous lesions from prostate tissue slides, according to the report.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
Additionally, breakthroughs in treatment have contributed significantly to the country’s decreasing cancer mortality rate. One of the main reasons that treatments are improving is because the medical community has gained a greater understanding of the human genome, according to Dr. Cohn.
“As we’ve sequenced the human genome, we have begun understanding some of the molecular genetic changes that occur within cancer, as well as how those molecular changes interact with their environments,” he said. “If you understand that there are significant mutations in a cancer, then you can develop drugs that target those specific mutations. Now, we have more directed treatments that can improve the chances of not dying of cancer.”
U.S. oncologists should prioritize the accessibility of genomic testing to lower cancer death rates, Dr. Cohn said. His team at the James Cancer Hospital is currently pursuing an initiative to ensure medical oncologists across the entire state of Ohio have the knowledge of and access to genomic testing. These tests can lead to more personalized and effective cancer care, but patients who do not live in urban centers still often lack access to this testing, he pointed out.
Advancements in cancer treatment also include a greater focus on immunotherapy, which Dr. Cohn said has the potential to “entirely change the paradigm of cancer treatment.” To him, leveraging the body’s own immune system against cancer cells is the fourth pillar of cancer treatment, following the more traditional treatment methods of drugging cancer with chemotherapy, damaging it with radiation, and removing it with surgery.
Immunotherapy in oncology refers mainly to the use of immune checkpoint inhibitors, which are therapeutics that release brakes on T cells. In 2011, the FDA had approved only one checkpoint inhibitor, ipilimumab, which is used to prevent melanoma from coming back. There are currently nine FDA-approved checkpoint inhibitors, according to the report.
To ensure that cancer mortality rates continue falling, the U.S. will have to tackle the obesity epidemic, Dr. Cohn declared. He pointed out that obesity and physical inactivity are risk factors that increase the risk of developing some of the few cancers that are experiencing rising incidence rates in the country, such as kidney and uterine cancers.
This ties in with social determinants of health, as many low-income Americans live in ZIP codes that lack accessible healthy food options. Efforts to further decrease cancer death rates in the U.S. must focus on addressing these social determinants, Dr. Cohn said. Factors such as a patient’s ability to pay for their care and geographical distance from a cancer treatment center still play a significant role in whether or not they survive cancer, he said.
“The country has invested substantially to get to a place where we have better outcomes for those who are able to access care,” Dr. Cohn said. “The next thing we should do is increase access for people who are not currently receiving that level of care, because the improved standard of care exists already.”
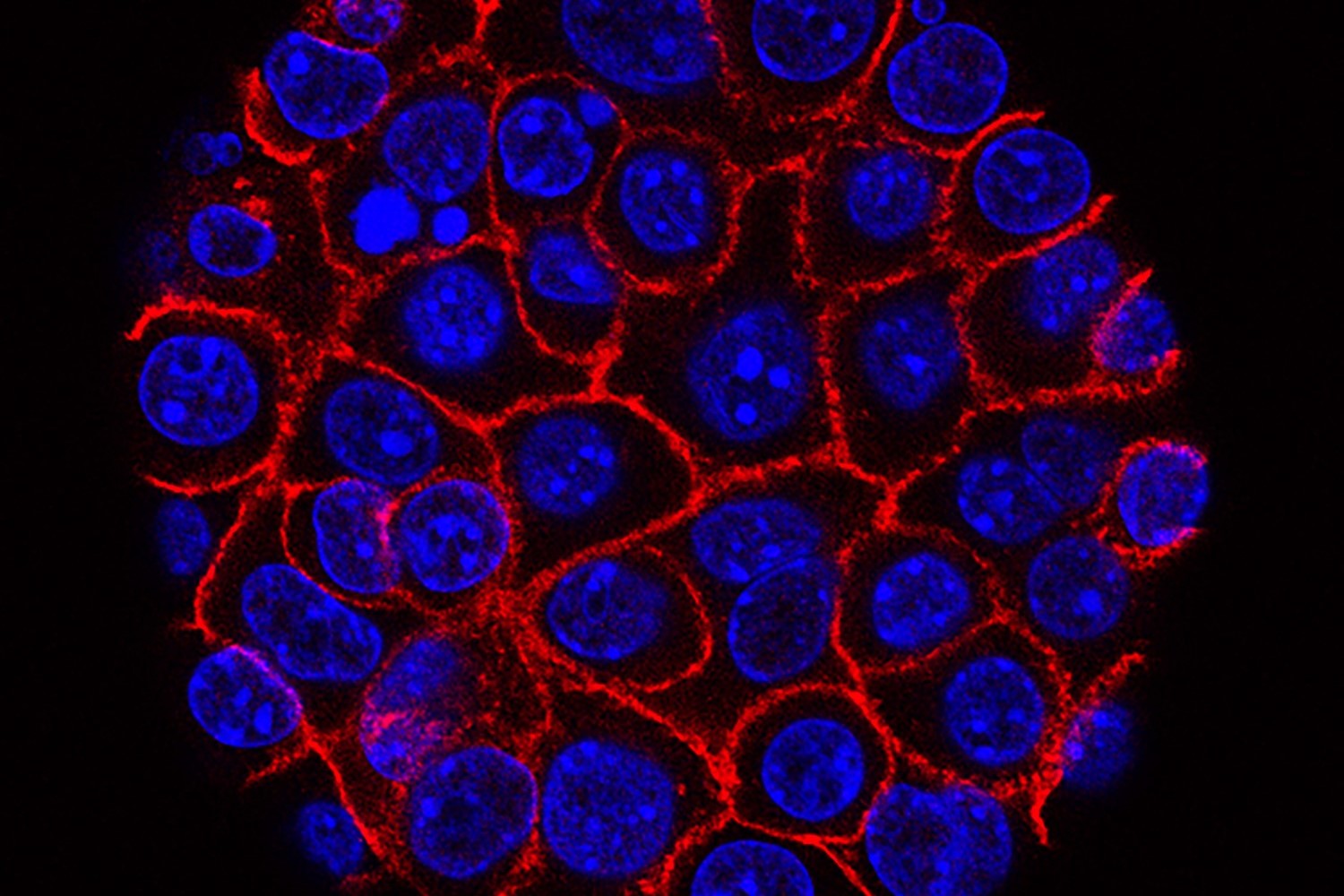
Photo: Public domain image from the National Cancer Institute












