A new proposal from the Centers for Medicare and Medicaid means that Medicare could cover CAR T-cell therapy as a treatment for cancer, dependent on specific patient safety and monitoring requirements.
Under the terms of the proposal released Friday, Medicare patients with relapsed or refractory cancers would be able to get coverage for CAR T-cell therapy if their clinic adheres to specific provisions including at least two years of patient monitoring after the treatment.

As Healthcare and Biopharma Companies Embrace AI, Insurance Underwriters See Risks and Opportunities
In an interview, Munich Re Specialty Senior Vice President Jim Craig talked about the risk that accompanies innovation and the important role that insurers play.
Hospitals or outpatient clinics administrating CAR-T therapy will also be required to enroll patients receiving treatment in a national audited registry to help study the effects of the therapy against the clinical trial results that led to regulatory approval of the treatments. CMS-approved clinical studies using CAR-T therapy would also be held to those same standards.
CMS said that data from the registries will be used to identify the kinds of patients that benefit from CAR T therapy and inform future coverage decisions.
The new CMS proposal builds on previous moves from the agency to support coverage of CAR T therapies. Last year, CMS agreed on reimbursement rates for CAR T through Medicare Part B, which largely covers outpatient medical needs.
The lack of an overarching CMS reimbursement policy, however, has meant that coverage decisions have generally landed on the desk of local Medicare Administrative Contractors.

The Power of One: Redefining Healthcare with an AI-Driven Unified Platform
In a landscape where complexity has long been the norm, the power of one lies not just in unification, but in intelligence and automation.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” CMS Administrator Seema Verma said in a statement.
“Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
CMS will have a final decision on the proposal within two months after the end the 30-day public comment period.
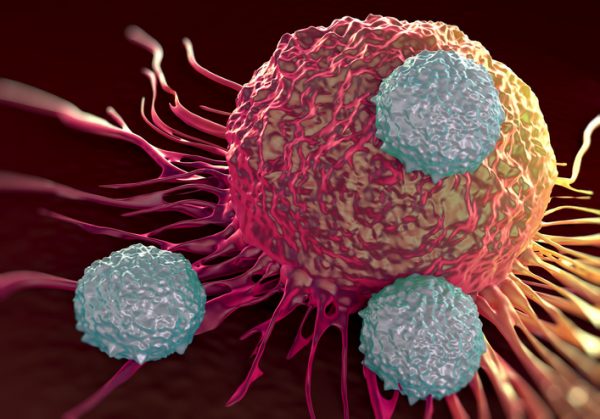
CAR T-Cell therapy – short for Chimeric Antigen Receptor T-Cell therapy – is a relatively new type of cancer treatment where clinicians re-engineer a patient’s T-Cells to target and destroy cancerous tumor cells.
The therapy has been hailed as revolutionary new treatment protocol for adult large B-cell non-Hodgkin’s lymphoma and recurrent childhood acute lymphoblastic leukemia.
The two FDA approved CAR-T treatments are Novartis’ Kymriah and Yescarta from Gilead Sciences are are priced at $475,000 and $373,000, respectively. The figures, however, don’t include potential costs incurred in the case of common and intense side effects like cytokine storms.
Those high prices have meant that payer organizations have generally been wary of reimbursement approvals for CAR-T treatments, even when considering their potentially clinical value to patients.
Most commercial payers cover CAR-T therapies largely on a case-by-case basis and reimbursement decisions can lag dependent on the level of sophistication of a particular patient’s insurer.
However, there has been increasing momentum for coverage with regulators like NICE, the U.K.’s drug pricing watchdog, recommending coverage for both Yescarta and Kymriah after negotiations with the drugmakers.
Photo: royaltystockphoto, Getty Images






