Healthcare’s holy grail of interoperability has long been an overarching priority for policymakers looking to leverage the untold data silo’d away in EHRs and other systems.
The U.S. Department of Health and Human Services under the Trump Administration has sought to promote this goal by empowering patients with a free flow of information to make better and more informed decisions about their care.
A new proposed rule from the Centers and Medicaid Services would require government health plans and health plans sold on the federal ACA exchanges to give patients free access and control over their health information by 2020.
The proposal would apply to the roughly 125 million patients on Medicaid, the Children’s Health Insurance Program, Medicare Advantage and health plans in the federal ACA exchanges.
CMS has long sought to advance policies meant to open up patient control of their healthcare data. The rule is a continuation of the organization’s MyHealthEData initiative, a program launched last year to give patients the power to access and share their healthcare information as a way to promote more informed consumer choice and improved care coordination.
Policymakers have already been pushing healthcare providers to open up access to patient health records through reimbursement policy, but this long-awaited proposal goes even further in pushing the ball forward.
“By outlining specific requirements about electronic health information, we will be able to help patients, their caregivers, and providers securely access and share health information. These steps forward for health IT are essential to building a healthcare system that pays for value rather than procedures, especially through empowering patients as consumers,” HHS Secretary Alex Azar said in a statement.
As part of the larger initiative to give patients more agency over their care, CMS is also looking at forcing providers and plans to adopt open data sharing technologies that will allow for the free exchange of data and ease the transition of patients from one plan to another.
A persistent record of diagnoses, procedures, tests and providers could provide better insight into a patient’s needs and situation and promote care coordination and improved health outcomes.
Last year, CMS launched a standardized API for Medicare fee-for-service plans, but is now looking to expand that effort to other government health plans by requiring programs to implement a HL7 FHIR-based API to open up data access to third party apps and developers.
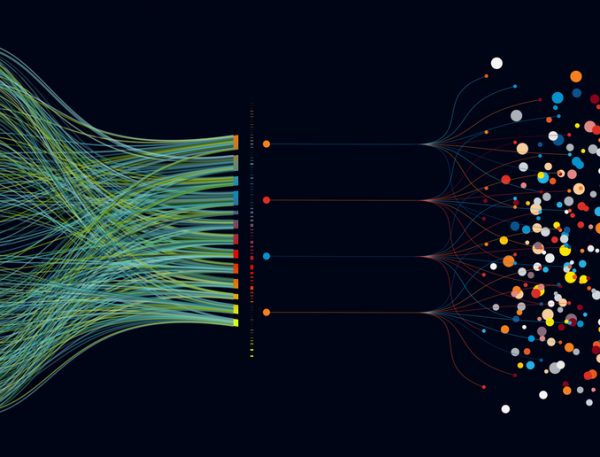
APIs essentially serve as software adapters allowing for efficient transfer of health information across a variety of systems. CMS is also proposing that this API be used to allow beneficiaries and potential plan enrollees to see provider networks to help them make decisions on care.
“This unprecedented step toward a healthcare future where patients are able to obtain and share their health data, securely and privately, with just a few clicks, is just the beginning of a digital data revolution that truly empowers American patients,” CMS Administrator Seema Verma, said in a statement.
Payers in the aforementioned programs would also be encouraged to join a “trusted exchange network” that would allow them to participate in nationwide exchanges of data to promote interoperability.
Those organizations who choose to limit the availability and disclosure of electronic health records will be publically reported for “information blocking” as a way to incentivise better behavior.
A separate – but related – proposed rule from by the Office of the National Coordinator for Health Information Technology goes into more specifics about how the government is seeking to promote better health information sharing and access through the adoption of standardized APIs.
Provisions of the rule include the adoption of the United States Core Data for
Interoperability as a standard for clinical data classes, as well as the required adoption of HL7 FHIR standards and implementation specifications meant to support API-enabled services.
Information blocking is also a key focus on the ONC rule, with additional requirements for health IT developers to ensure that they don’t take actions which inhibit the exchange access and use of health data. Certain exemptions to the information blocking rule were also laid out including preventing harm, promoting privacy and security of electronic health information and recovering costs reasonably incurred.
Additionally, ONC is seeking comments on what pricing information should be included in EHR data to inject more pricing and cost transparency into the industry.
“By supporting secure access of electronic health information and strongly discouraging information blocking, the proposed rule supports the bi-partisan 21st Century Cures Act. The rule would support patients accessing and sharing their electronic health information, while giving them the tools to shop for and coordinate their own health care,” said ONC National Coordinator for Health IT Don Rucker, in a statement.
Picture: shuoshu, Getty Images










