The Covid-19 pandemic has impacted the quality of care, access to healthcare providers, and driven a greater demand for mental health professionals than ever before in modern medicine. To slow the spread of Covid-19 and address the demand for acute care due to the number of Covid-19 cases, maintenance and surveillance care overall was delayed or abandoned between March 2020 and March 2021 leading to the current backlog of undertreated patients.
Mental health has a surge in need

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
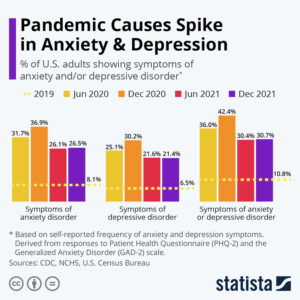
The greatest Covid-19 associated healthcare need is mental health. Country statistics have proven that the pandemic related impact on lives, daily living and quarantine has created the greatest demand for mental health professionals. There is currently a shortage of mental health professionals, limiting the time that can be spent with each patient, as well as long waiting lists for care. Click image to enlarge.
In cases where medication can help ease or address immediate mental health disorders, trial and error isn’t the most effective way to find the best therapy. Only four out of ten people treated with antidepressants improve with the first medication they are prescribed. Mental health providers and patients do not have the time or luxury to cycle through prescription treatments to find a treatment that addresses the unique needs of the individual patient. Mental health professionals and patients need efficient solutions to point to the medications that they know will work from the start.
Precision prescribing, a new clinical trend that brings together the patient’s relevant data points such as current medical conditions and comorbidities, liver and kidney function, previous medications, and drug interactions, also considers the genomic make-up of the patients, or their pharmacogenetics profile. Pharmacogenetic (PGx) testing can help by assessing a patient’s genetic profile to understand how likely they are to respond to a medication—from the start or if they will develop a side effect. PGx testing for psychiatric medication is currently available for medicines designed to treat bipolar disorder, depression, obsessive-compulsive disorder (OCD), schizophrenia, and more. In some advanced clinics, for some specific conditions, and in some specific medication uses, using such modern tools to incorporate pharmacogenetics into the decision process is a preferred standard of care.
How precision medicine for mental health works
Most antidepressants/antipsychotics are metabolized by enzymes in the liver. Because of the strong relation between pharmacogenetic variants and enzymatic activity, analysis of key enzymes has been an early focus for the clinical use of PGx in psychiatry.
For example, in one study the rate of response to initial antidepressant treatment was only 49.6%, and a systematic review showed that non-responders to one or more treatments have a 15% likelihood of suicide ideation compared to 6% of patients with treatment-responsive depression and 1% in the general population (Mrazek et al., 2014).
Additional studies have shown that up to 43% of patients with major depressive disorders may discontinue antidepressants due to treatment-emergent adverse effects. A major determinant of emergent side effects and lack of efficacy is the relation between dosage and systemic exposure to the drug.
There are two key challenges to optimize the utility of PGx testing for precision prescribing:
- The testing outcome and information must be available at the point of care, and
- This information must be provided in an efficient and actionable manner for truly personalized care.
A precision prescribing platform could greatly alleviate some of the challenges created by the shortage of mental health professionals; improve patient treatment, safety, and satisfaction; and ease the financial burden on the healthcare system.
How to implement precision prescribing into your healthcare system
There are several testing companies that provide PGx testing, however implementing a platform that provides evidence-based precision medication management at the point of patient care is likely to have the greatest utility and optimize efficiency in care.
While most providers currently practice reactive medicine, a shift to predictive medicine enhanced by PGx could help patients reach greater success in managing mental health issues. There is technology now available to predict how a patient may respond to treatment or what is the risk of developing a disease. When this PGx data is considered along with other well-known factors that influence how an individual will respond to a medication, such as kidney function, liver function, comorbidities, and so on, it can help clinicians determine a personalized plan to avoid or delay the onset of diseases or complications related with the conditions or treatments.
Leveraging a precision prescribing platform with embedded genomic analysis will help physicians improve care and reduce costs by providing valuable information to inform mental health medication choices that can deliver treatment success for their patients from the start. This would fundamentally disrupt and digitally transform the centuries-old approach to prescribing, trial and error, to one of efficiency and accuracy at a time when we need it most.
Photo: Wacharaphong, Getty Images
Sara Rogers, PharmD, BCPT, is the Cofounder and Director of Clinical Affairs at the American Society of Pharmacovigilance (ASP), an organization with the goal to rapidly and dramatically reduce the high rate of adverse drug events (ADEs) in the US. She co-chairs the Pharmacogenomics Access and Reimbursement Coalition (PARC) to address pain issues and the barriers posed for widespread implementation of pharmacogenetic testing, a proven tool for proactively addressing medication side effects. Sara also co-developed the Standardizing Laboratory Practices in Pharmacogenomics (STRIPE) initiative, a public and private multidisciplinary collaborative community to accelerate the development of personalized medicine practices as a standard of care.