
History has shown that while healthcare is more open to adopting technology to improve outcomes, bureaucracy, ego, money, or indifference to change still tend to get in the way. Technology is not our only problem unfortunately, healthcare has so many more. In this article, I put together some statistics that show we still have a long way to go to make healthcare more accessible to everyone.
Here are the 25 shocking statistics that keep healthcare executives up at night.

As Healthcare and Biopharma Companies Embrace AI, Insurance Underwriters See Risks and Opportunities
In an interview, Munich Re Specialty Senior Vice President Jim Craig talked about the risk that accompanies innovation and the important role that insurers play.
- Medicare reimbursements declined by 9%
The Medicare Payment Advisory Commission found that hospitals experienced a -8.5% margin on Medicare services in 2020, and it projects that margin will fall to -9% in 2022. Combined underpayments from Medicare and Medicaid to hospitals were $100 billion in 2020, up from $76 billion in 2019.
- 46% of Federally Qualified Health Centers are troubled by rising competition
CEOs of federally qualified health centers do not feel equipped to manage revenue cycle issues stemming from growing competition. About 61 percent of leaders at federally qualified health centers (FQHCs) anticipate competition to rise in the next year, threatening their revenue cycle and financial stability, a recent Sage Growth Partners (SGP) survey revealed.
The survey of 175 FQHC CEOs uncovered that almost one-half (46 percent) of health centers face competition from other FQHCs.
But FQHCs are also competing against healthcare organizations with greater economies of scale for pricing services and larger budgets for provider compensation. A little over one-half of urban and rural health centers stated that they face competition from urgent care and hospital-based ambulatory care sites.
- Medical errors are now the third leading cause of death in the U.S.
Johns Hopkins Hospital published a comprehensive study on medical errors that estimated 250,000 deaths per year occur as a result of medical errors.
- 12 million diagnostic errors are expensive, costing $750 billion per year
All told, diagnostic errors affect an estimated 12 million Americans each year, and likely cause more harm to patients than all other medical errors combined, with the most common among them missing early cancers and heart diseases, which cost over 100,000 lost lives and $750 billion.
Patient safety advocates have long sought to make a “business case” to demonstrate that if healthcare organizations invest in safer practices and systems, they will reap financial returns in the form of reduced malpractice costs and other expenses.
- 42% of physician staff are burnt out
Knowing my friends in the space, and that I have yet to see them for almost 2 years paints the picture perfectly. With Covid, double shifts, and staffing concerns, 42% of physicians reported they are burnt out, and finding little time to relax and enjoy life. I never see my primary care doctor friends given their battle against time. When I do get to see my friends it is usually due to them leaving healthcare completely and focusing on building a new startup which is great, but where are the incentives to stay and clinically help patients? Those incentives are slowly dissipating.
- 92% of U.S. physicians admit to making some medical decisions based on avoiding lawsuits
This startling statistic came from a 2010 Jackson Healthcare study. on defensive medicine. The study also found that clinicians from other countries, including New Zealand, Canada, the United Kingdom, and Sweden did not report any ordering of unnecessary tests, treatments, or consultations to avoid lawsuits.
- 58% of clinicians felt unsafe about speaking up about a problem they observed or were unable to get others to listen
This statistic first appeared in a 2005 report called “Silence Kills.” The report also found that “84 percent of doctors observed colleagues who took dangerous shortcuts when caring for patients and 88 percent worked with people who showed poor clinical judgment.” And “less than 10 percent of physicians, nurses, and other clinical staff directly confronted their colleagues about their concerns.”
- $765,000,000,000, or 30% of all U.S. healthcare costs, each year is wasted
Institute of Medicine (IOM) study found that of the $2.5 trillion spent on domestic healthcare costs in 2009, $765 billion (or 30%) was attributable to preventable costs such as fraud, unnecessary services, inefficiently delivered services, and excessive administration costs. At this rate, healthcare costs will skyrocket to an unsustainable $4.5 trillion in 2019.
- Medicare and Medicaid pay less than the cost of caring for program beneficiaries – a shortfall of $75.8 billion in 2019 born by hospitals
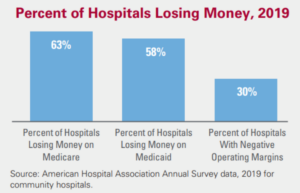
Image source : American Hospital Association Annual Survey
America’s hospitals are faced with mounting financial challenges. Government programs like Medicare and Medicaid pay hospitals less than the cost of caring for the beneficiaries these programs cover while insurance companies negotiate deep discounts with hospitals.
The growing numbers of the uninsured and underinsured further complicate this financial picture. While there are government programs such as Medicare and Medicaid that disproportionately use hospital payments designed to help hospitals with the cost of treating low-income and uninsured patients, it are not enough to cover the cost of care.
In 2019, Medicare and Medicaid underpaid U.S. hospitals by $75.8 billion, meaning hospitals received only 87 cents for every dollar they spent caring for Medicare patients and only 90 cents for every dollar they spent caring for Medicaid patients. The data precede and do not reflect the impact of the Covid-19 pandemic.
Noting that 63% of hospitals lose money on Medicare.
- Hospitals provided $41.6 billion in uncompensated care, both free care and care for which no payment is made by patients, in 2019.
Hospitals in 2019 provided $41.6 billion in uncompensated care, meaning care for which no payment was received from the patient or insurer, according to the latest data from the AHA’s Annual Survey of Hospitals.
Uncompensated care is the sum of a hospital’s bad debt and the financial assistance it provides. It does not include other unfunded costs of care, such as underpayment from Medicare and Medicaid, or account for other services and programs that hospitals provide to meet identified community needs.
- 22 percent of FQHCs are starting to consider alternative payment models, but payers aren’t changing reimbursement yet
Almost a quarter (22%) of FQHCs say they could move to value-based reimbursement in less than six months if a major payer changed its reimbursement model. Sixty-eight percent say it would take 7-24 months, and 10% say it would take more than 24 months. FQHC leaders are experiencing a continued downward trend for fee-for-service, and an upward trend for alternative payment models.
- Large self-insured employers lack power to effectively negotiate hospital prices
Fifty-five percent of Americans younger than 65 years receive their health insurance from their employers. Recently, hospital prices paid by employers have increased much faster than inflation and outpaced what public payers pay. The price differential paid by employers for hospital services increased from 10% above the Medicare rate to more than 100% above the Medicare rate in many metropolitan statistical areas (MSAs) between 2005 and 2019.
If the differential between public- and private-sector prices continues to widen, it could continue to cause slower or negative effective wage growth for US workers, whose total compensation increases have been absorbed by more expensive health benefits. In most areas of the United States, self-insured employers lack the market power to negotiate hospital prices. There is no evidence that greater employer market power is associated with lower hospital prices in the employer-sponsored insurance markets.
- 25% of FQHCs find it challenging to manage their marketing goals
Twenty-five percent of large FQHCs who report not having a marketing plan also report that they find financial sustainability extremely challenging. Sixty-two percent of respondents say marketing is extremely important to achieving their organization’s growth goals. Yet less than one-quarter (23%) report having a fully implemented marketing plan.
- Hospital CEOs face financial challenges in 2022
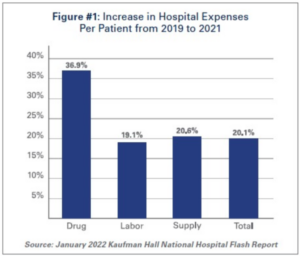
Image Source: January 2022 Kaufman Hall National Hospital Flash Report
A new AHA report highlights the significant growth in expenses across labor, drugs, and supplies (see chart), as well as the impact that rising inflation is having on hospital prices.
According to data from the Bureau of Labor Statistics, hospital employment is down approximately 100,000 from pre-pandemic levels. At the same time, hospital labor expenses per patient through 2021 were 19.1% higher than pre-pandemic levels in 2019.
Labor costs account for more than 50% of hospitals’ total expenses. Therefore, even a slight increase in these costs can have significant impacts on a hospital’s total expenses and operating margins.
- 55-65% of referrals are sent to out-of-network providers costing health systems millions
When it comes to referrals, 55-65% are sent to out-of-network providers. This occurs because typically, providers, referring physicians, and call centers lack information about the specialists to which they are referring patients. This lack of information can add up, costing upwards of $821,000-$971,000 per physician. However, one in four healthcare systems don’t know or even track how much revenue they are losing on referral leakage. It is estimated that the average hospital loses 10-30% of its revenue to patient leakage. These costs can skyrocket over time as physicians lose chances to coordinate care for patients within their networks.
- 518 hospital executives have left their jobs from January to April 2022
Top executives in all businesses are stepping away at a much higher pace than in previous years, and that’s being seen at hospitals as well. From January through April 2022, 518 chief executive officers have left their positions, according to a new report by Challenger, Gray & Christmas, Inc., a business coaching and outplacement firm. That’s the highest total from January through April since the firm began tracking CEO exits in 2002. It’s an 18% uptick from the same four-month period in 2021.
Through April, 36 hospital CEOs have left their posts, up from 20 chief executive departures over the first four months of last year. That represents an 80% increase. Among pharmaceutical companies, 10 chief executives have left between January and April 2022, compared to just three in the same period a year ago. Leaders at healthcare companies were a little more likely to stay in their posts than a year ago, according to the report. Through April, 46 healthcare CEOs exited their positions, compared to 63 in the same span of 2021.
- Expensive EHRs cost ranges from $15K to $70K per provider, and may not be the correct choice, choose wisely.
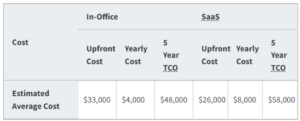
Image Source: https://www.healthit.gov/faq/how-much-going-cost-me#footnote-1
Several studies estimate the cost of purchasing and installing an electronic health record (EHR) ranges from $15,000 to $70,000 per provider. Costs vary depending on whether you select an on-site EHR deployment or a web-based EHR deployment. Web-based EHR deployment, known as Software as a Service (SaaS), typically requires providers to pay a fixed monthly subscription cost. On-site deployment typically requires providers to pay for ongoing costs to support and manage on-site data servers.
The following chart from the Michigan Center for Effective IT Adoption provides the estimated average upfront cost, yearly cost, and five-year total cost of ownership (TCO) for on-site and SaaS EHR deployments. These cost estimates are based on the experiences of Regional Extension Centers (RECs) in the field.
Jeff Riggins, health IT expert and digital media consultant at Drury University, sums up the issues with current EMRs quite well:
“Sadly, most EMR software is terribly inadequate. They were built on obsolete platforms with little thought dedicated to user experience. Most EMR packages started as billing systems slowly adding clinical components to gain market share. The design phase was largely overlooked as the functionality of the system was all the government had created guidelines for. This is why physicians complain they have to click 30 times to give a patient a sleeping pill.”
Once you are locked in, it is very hard to switch, the absorbent cost of implementation and training prevents most systems from leaving their EHR vendor until many years later, if ever.
- Approximately 43.1 million patient records were breached in 2021
The rise of digitization in healthcare, heavily fueled in the U.S. in recent years by incentives of the outgoing administration, has brought an unintended and treacherous side-effect: vulnerability to the increasingly rampant hacking of healthcare data.
The HHS website data confirms the near-exponential increase in cybercrimes resulting from healthcare data breaches. At least 526 of the 713 breaches reported in 2021 were categorized as Hacking/IT Incidents at HHS.gov “Wall of Shame”.
These incidents accounted for 94 percent of total records breached – a staggering 43.1 million records in 2021.
Healthcare providers and business associates seem to be getting the message regarding encrypting and protecting electronic devices and computers. Only 16 of these breaches affecting less than 100,000 patients were reported in 2021. This represents a dramatic reduction from years past when lost or stolen devices were one of the largest contributing factors to healthcare data breaches.
- 96 percent of online complaints about doctors are about their customer service
A nationwide study has uncovered what drives patients to write glowing, or scathing, reviews on the Internet. For a study of online doctor reviews coast to coast, Vanguard Communications developed special software to analyze Google+ reviews of doctors, group medical practices, clinics, and hospitals.
The software analyzed 34,748 patients’ reviews of their physicians throughout the United States and determined that customer service is the leading distinction between highly rated and poorly rated doctors.
After compiling data containing the words patients used in describing their experiences with medical practices, the software determined the most common phrases associated with each review star level. An analysis of these most common phrases revealed that an incredible 96 percent of patient complaints are customer-service related, while a mere 4 percent complain about the quality of care or misdiagnosis.
- 30% of all medical malpractice claims result from communication failures
Nearly one-third of national medical malpractice complaints involve some form of communication failure, according to the report “Malpractice Risks in Communication Failures” from CRICO.
In 23,658 of the malpractice cases filed between 2009 and 2013, 30% of these cited some form of miscommunication, either between providers or between the provider and the patient. The report examined communication breakdowns with a focus on general medicine, obstetrics, nursing, and surgery in order to offer healthcare providers and leaders insights on how to improve skills and systems and how to mitigate risks.
“An important takeaway from this analysis is that when a claim has provider-provider communication failures, it is more likely to result in payment than cases with provider-patient communication issues,” Mark E. Reynolds, president of CRICO, said in a statement.
- Medicare punishes 2,499 hospitals for high readmissions
The federal government’s effort to penalize hospitals for excessive patient readmissions is ending its first decade with Medicare cutting payments to nearly half the nation’s hospitals.
In its 10th annual round of penalties, Medicare is reducing its payments to 2,499 hospitals, or 47% of all facilities. The average penalty is a 0.64% reduction in payment for each Medicare patient stays from the start of this month through September 2022. The fines can be heavy, averaging $217,000 for a hospital in 2018, according to Congress’ Medicare Payment Advisory Commission, or MedPAC. Medicare estimates the penalties over the next fiscal year will save the government $521 million. Thirty-nine hospitals received the maximum 3% reduction, and 547 hospitals had so few returning patients that they escaped any penalty. Look up if your hospital is being penalized.
- 43% of Community Health Centers operate on negative margins
Like other health care providers during the pandemic, community health centers have seen non-Covid revenue plummet. Health centers may be especially vulnerable because they are located in very poor communities and serve vulnerable populations, which together cause them to operate under serious economic constraints. These constraints show up in narrow operating margins (a concept that reflects a comparison of costs against revenue available). Experts recommend a margin of 2.5 percent for hospitals.
Between 2008 and 2011, hospitals reported a median operating margin of 2 percent for health centers, but one in four reported negative operating margins. According to our calculations using the 2018 Uniform Data Set, 56 percent of health centers had operating margins of less than 2.5 percent and 43 percent had negative margins. Approximately 16 million (or one in two) health center patients are at immediate risk of losing access to care.
- 68% scored personnel shortages as a very significant problem of (5) on a scale of (1 to 5)
Community hospital CEOs responding to the Personnel Shortages Survey were asked to rate how significant personnel shortages were to the hospitals they led on a scale of 1 to 5, where 1 was “Not at all Significant” and 5 was “Very Significant.” The majority, 68%, scored the issue as significant, that is, gave a score of 4 or 5. A small proportion of CEOs, 12%, rated the significance of personnel shortages in their hospitals as a 1 or 2. Survey respondents were asked to list the types of personnel who posed the No.1, No. 2, and No. 3 challenges to their hospitals with respect to staffing shortages. Bringing the data together, Table 1 shows the proportion of CEOs who named the staff listed among their top three personnel shortages.
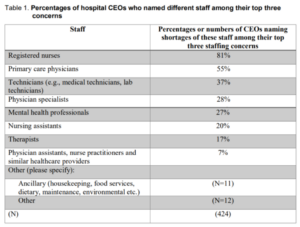
Image Source: ACHE.org
- Cost of preventable medical harm in healthcare is a whopping $58,776 per injury
Data indicate that hospitals, on average, externalize 78 percent of medical costs associated with all injuries and 70 percent of medical costs associated with negligent injuries to patients through medical billing and malpractice claims. The average cost per incidence of preventable harm is approximately $58,776 per injury. Increasingly, Medicare and other insurers will not cover the cost of medical treatment related to adverse events and the remaining costs are typically externalized through malpractice insurance, which costs an average of $123 per patient the hospital sees.
But who pays for the remaining $83 billion in indirect costs? The patients themselves typically shoulder costs and the economy at large also suffers through disability payments, lost productivity, and other associated costs. Many patient safety advocates have voiced concerns that hospitals are responsible for such a small proportion of preventable harm costs. Advocates argue that hospitals should be accountable for more of the expenses associated with medical errors, which would lead to safer systems and practices. Essentially, this makes high-quality patient care a “business case” where more precise care would reduce malpractice and other costs.
- Hospital discharge and readmission costs health systems $20 billion annually
Discharging patients from the hospital is a complex process that is fraught with challenges and involves over 35 million hospital discharges annually in the United States. The cost of unplanned readmissions is 15 to 20 billion dollars annually. Preventing avoidable readmissions has the potential to profoundly improve both the quality of life for patients and the financial well-being of health care systems.
Researchers in the field of Transitions of Care evaluate the effectiveness of various approaches to improve the discharge process. One classification scheme to categorize these interventions is to consider them as pre-discharge interventions (patient education, discharge planning, medication reconciliation, scheduling a follow-up appointment); post-discharge interventions (follow-up phone call, communication with ambulatory provider, home visits); and bridging interventions (transition coaches, patient-centered discharge instructions, clinician continuity between inpatient and outpatient settings).
Conclusion:
I have been in healthcare for well over 20 years and love it. I enjoy everything about it, my colleagues, partners, and teammates, but I can tell you it is hard. While navigating all the landmines that business uncovers, it’s amazing what people can come up with to make a difference for all Americans that deserve a better life and health.
In the current state of preventive screening, primary care is not well trained in the art of managing chronic disease care which is why Americans are dying at an astounding rate. Our goal should be to not only to find eligible patients using advanced machine learning tools, but contact the patient with our dedicated care team, help patients get to the imaging center, read the scan via our AI-enabled radiology screening platform, and ensure the patients come back year after year (which is the most important part). This is the only way to effectively help vulnerable patients that need these life-saving screenings.
You can be a part of the change.
Photo: VioletaStoimenova, Getty Images
Jonathan Govette is the Co-Founder at Oatmeal Health, an AI-enabled teleradiology and patient engagement service that coordinates lung cancer screenings for underserved, vulnerable patients.
Oatmeal Health is a veteran-owned and clinician-led platform changing how self-insured employers, FQHCs, and payers manage population risk and improve outcomes.
Through its discovery of novel AI systems, the company is enabling the full potential of its platform to identify high-risk patients early and intervene with screenings before their health worsens so healthcare costs don't spiral out of control while delivering a better experience to families, employers, clinicians, and health plans.
Jonathan received his B.S. from California Polytechnic University in San Luis Obispo, He developed optimal referral pathways and created the first-of-its-kind referral management platform in 2010. Jonathan was selected as the winner of Samsung's Digital Health Conference, a finalist in Venturebat's Health Beat Conference, and a Techstars / Cedar Sinai Alumni.
Trusted healthcare technology expert quoted in Forbes Magazine, HIMSS, Medcity News, Beckers Healthcare, Newsweek, Techcrunch, Modern Healthcare, and others. Collaborations with Cleveland Clinic, Harvard Medical, and AARP.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.








