A rare immunodeficiency discovered just 10 years ago now has its first treatment. The FDA has approved a Pharming Group drug developed to treat activated phosphoinositide 3-kinase delta syndrome, or APDS, a disease that leads to low levels of white blood cells that fight pathogens and prevent infection.
The FDA said Friday that its approval of the drug, lenolisib, covers adults as well as children 12 and older who have APDS. Leiden, Netherlands-based Pharming will market its new twice-daily pill under the name “Joenja.”
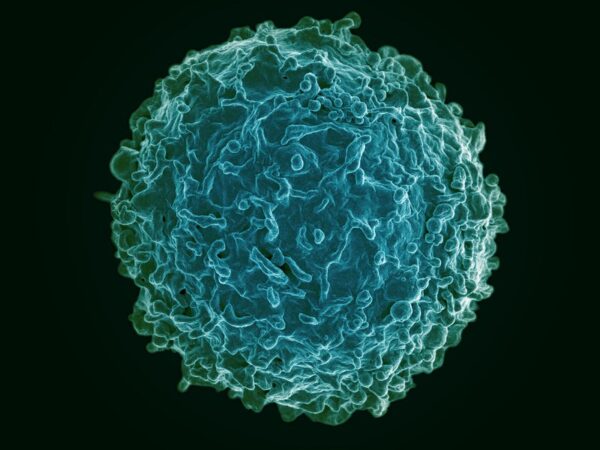
APDS is caused by mutations to genes that encode PI3KD, a protein key for normal development and function of white blood cells. The disease particularly affects B and T cells, resulting in cells that improperly mature and malfunction. The disorder makes patients more susceptible to recurrent infections in the sinuses, ears, and respiratory tract. It may also lead to enlarged lymph nodes, tonsils, spleen, and other organs, which can obstruct the airways and gastrointestinal tract. Furthermore, this protein deficiency also makes patients more prone to developing blood cancers.
The overlapping symptoms of primary immunodeficiencies lead to APDS frequently being misdiagnosed. The disease was first characterized in 2013 and can now be diagnosed with genetic testing. According to Pharming, APDS affects an estimated 1 million to 2 million people worldwide. Treatment has consisted mainly of symptom management: prophylactic antibiotics, immunoglobulin replacement, and immunosuppression. If lymphomas develop, chemotherapy and stem cell transplants are treatment options, but these treatments introduce new complication risks.
Joenja is a small molecule designed to block the PI3K-delta protein, an approach intended to inhibit signaling pathways that lead to dysregulation of B cells and T cells. FDA approval of the drug is based on a placebo-controlled Phase 2/3 study that enrolled 31 adults and children 12 and older with a mutation PI3K-delta mutation. The FDA said results showed that by day 85 of the study, patients in the Joenja group showed a reduction in the size of their lymph nodes and normalization of their levels immune cells, as measured by calculating the percentage of naïve B cells out of total B cells, indicating improvement.
Pharming already has one FDA-approved product, the hereditary angioedema drug Ruconest. In 2021, that drug accounted for €198.8 million in revenue, down 9% from the prior year. Pharming licensed Joenja from Novartis in 2019, paying $20 million up front. The two companies partnered on Phase 2/3 testing. An additional $200 million is tied to the achievement of regulatory and sales milestones. Novartis is also entitled to receive royalties from Pharming’s sales of the new drug.

The Power of One: Redefining Healthcare with an AI-Driven Unified Platform
In a landscape where complexity has long been the norm, the power of one lies not just in unification, but in intelligence and automation.
FDA approval of Joenja comes with a priority review voucher (PRV) that entitles Pharming to receive speedy review of a future rare disease drug. Pharming said that according to the terms of the company’s license agreement with Novartis, the pharmaceutical giant has the right to purchase this voucher “for a small minority share of the value of the PRV.”
Pharming has scheduled a Monday, 8 a.m. Eastern time conference call to discuss Joenja’s approval.








