An Octapharma drug already sold in Europe and Canada for reversing the effects of blood-thinning medicines in patients undergoing emergency surgery or invasive procedures is now approved for use in the U.S. However, more complications and fatalities were observed in the study drug group, so as a condition of approval the FDA is requiring Octapharma to conduct additional post-marketing testing.
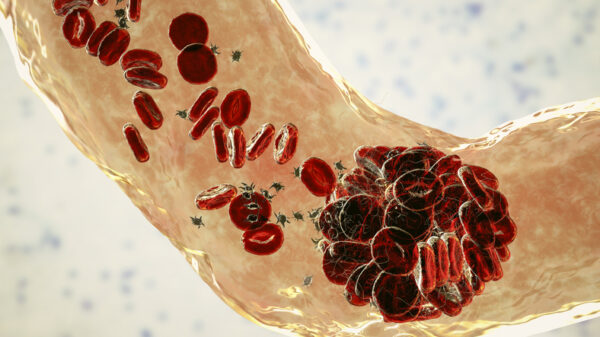
The drug, Balfaxar, is comprised of coagulation proteins derived from human plasma. It’s intended to counteract the effect of the blood-thinning drug warfarin. Warfarin and similar drugs are widely used to prevent blood clots after a heart attack or heart valve surgery. These drugs are also prescribed to prevent deep vein thrombosis, pulmonary embolism, and to lower the risk of stroke in people who have atrial fibrillation. But warfarin increases the risk of bleeding, which is a serious complication risk during surgeries.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
The portfolio of privately held Octapharma spans products derived from human plasma and human cell lines. Balfaxar, which is marketed as Octaplex in Europe and Canada, comes as lyophilized powder that must be reconstituted in a diluting agent. This reconstitution happens in an Octapharma device. The drug is administered intravenously and is intended to rapidly increase blood levels of key clotting factors and antithrombotic proteins.
The FDA based its approval on results from a double-blind Phase 3 clinical trial that compared Balfaxar to four-factor prothrombin concentrate (4F-PCC), a lyophilized concentrate of at least four coagulation factors. Results showed the Octapharma drug was roughly comparable to Kcentra, a 4F-PCC product marketed by CSL Behring. Balfaxar was effective in stopping bleeding in 94.6% of patients. By comparison, bleeding was stopped in 93.5% of patients treated with Kcentra.
While safety was similar across the treatment arms, more complications were observed in those treated with Balfaxar. Four deaths were reported in the Balfaxar group between 22 days and 45 days after surgery. One additional death occurred on day 47, which was after the study reporting period. None of the deaths were deemed to be related to the study treatment. In the Kcentra arm, one death was reported 10 days after treatment. The trial results also showed that three study participants treated with the Octapharma drug experienced four thromboembolic events. One of them was assessed as being possibly related to the study drug. No such problems were reported in the control arm, where patients received Kcentra.
The risk of serious and potentially fatal arterial and venous thromboembolic complications is highlighted in a black box warning on Balfaxar’s label. In the FDA’s approval letter to Octapharma, the regulator said it’s not enough for the company to conduct an analysis of serious post-marketing adverse events to assess these thromboembolic risks. The agency is requiring a post-marketing study that must enroll a minimum of 3,574 patients. Octapharma must submit the trial protocol to the FDA by the end of this year and complete the study by the end of 2031.
Octapharma, which is based in Lachen, Switzerland and has U.S. operations in Paramus, New Jersey, said it will meet the FDA’s requirement with two additional Phase 3 studies that are currently recruiting patients.
“The FDA approval of Balfaxar establishes a new therapy for medical providers when their patients need a 4F-PCC product,” Octapharma USA President Flemming Nielsen said in a prepared statement. “Octapharma is committed to providing patients with life-saving and life-enhancing therapies for critical care medicine.”
Illustration by Micro Discovery via Getty Images














