Spinal maladies are one of the U.S. healthcare system’s biggest burdens. Millions of Americans suffer from chronic lower back pain, but they rarely receive the holistic, long-term care they need to effectively treat this problem. Instead, chronic back pain is often mis-addressed through costly surgeries, such as a spinal fusion. This procedure can cost more than $100,000, but it often fails to do a good job of actually making the patient healthier, argued Commons Clinic CEO Nick Aubin. In an interview, he said that 40-50% of spinal surgeries “just don’t need to happen.”
This issue is what led Aubin to found Commons Clinic in 2021. The physician group, which has raised $34 million in funding, provides hybrid, value-based musculoskeletal care for patients in the Los Angeles area.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
“The one-liner here is that we’re building the Oak Street Health — or enter your favorite risk-based delivery model here — for multispecialty care, with an initial focus on the musculoskeletal stack. That’s spine, orthopedics, interventional pain management and physical therapy — the full spectrum — with ambitions to move into cardiology and a number of other interventional specialties,” Aubin explained.
Commons Clinic’s mission is to build innovative new care models that keep patients healthier for longer and bend the musculoskeletal cost curve. To further advance this mission, the startup announced on Wednesday the launch of its Center for Spine Economics, Outcomes & Research.
Through the center, Commons Clinic will establish a program for spinal restoration focused on motion preservation, minimally invasive procedures and biologic treatments. The company said it will invest $100 million in the center over the next 10 years, with the goal of making ambulatory spinal care delivery less expensive and more efficacious.
“The big boy hospital systems, like Cedars-Sinai or Sutter Health, have really used their market positioning and their hospitals as gravitational forces to consolidate specialty care markets. They bring physicians in, really ultimately focused on driving exorbitantly high facility fees at the expense of innovating on new care models that can make a big difference in communities,” Aubin declared.
The new center — which will have its main facility in Marina Del Rey, California — will research and test new models that move care out of the hospital and into community-based accountable care networks, he noted. Its programming will be led by two Commons Clinic physicians, Drs. Hyun Bae and Sanjay Khurana.
The center will include a technology lab designed for researchers to develop and validate new surgical techniques, devices, biologics, robotics, software applications and virtual intervention models. It will also involve a “payment innovation coalition” dedicated to creating new payment models and patient advocacy policies. The goal of this coalition is to establish prospective, full-risk bundled payments and consumer price transparency standards to help get more health plans and orthopedic physician platforms on board with Commons Clinic’s vision for improved spinal care.
Additionally, Commons Clinic aims to publish real-world evidence and open-source data showing the benefits of value-based spinal care models and the innovations developed within the center. The startup eventually hopes to partner with device manufacturers, pharmaceutical companies and other industry players to further this research and hopefully spearhead new products and interventions to make spinal care less invasive and more successful.
The center will also include a post-fellowship training program to prepare young physicians to thrive in value-based musculoskeletal care models.
Aubin pointed out that many musculoskeletal physicians have spent their entire careers practicing in high-cost hospital environments. They never really had a toolkit to deliver high value, lower cost care in an ambulatory environment, he said.
“We really feel like we can train that next generation of surgeons on the right care in the right setting with the right incentives,” Aubin remarked.
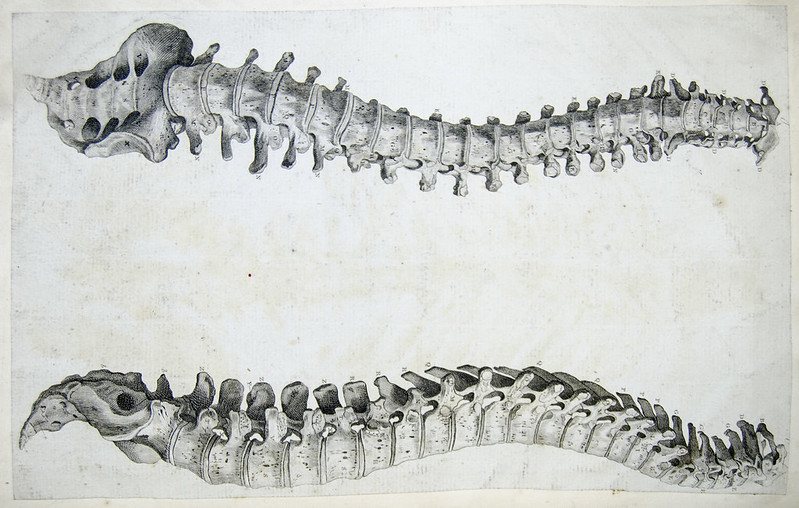
Photo: University of Liverpool Faculty of Health & Life Sciences via Flickr