The annual San Antonio Breast Cancer meeting drew clinicians and researchers for a few days at the end of 2023 to discuss advances in the field. While the past several decades have seen progress in early detection, recent innovations in metastatic breast cancer—or cancer that has spread to distant parts of the body, including the bone, brain, or lungs—continues to cause excitement. In the US, around 40,000 women and 4,000 men are diagnosed annually with metastatic breast cancer, and around 200,000 Americans are living with advanced disease.
But nearly 300,000 US citizens are diagnosed with breast cancer annually, and the specter of this non-metastatic disease converting to metastatic disease amplifies the weight of this issue. Two thirds of all breast cancer patients have a type of breast cancer called hormone receptor-positive (HR+). For these patients, a key part of treatment has been reducing the activity of hormones like estrogen, which fuel the growth of cancer cells. In 2017, the standard treatment approach changed to include the use of one of three drugs called CDK4/6 inhibitors – abemaciclib (brand name: Verzenio), ribociclib (brand name: Kisqali), or palbociclib (brand name: Ibrance). These drugs are used alongside other medications that modify hormone levels, such as letrozole or fulvestrant.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
These drugs have improved both PFS (progression free survival or the time until disease starts to grow again) as well as the overall survival of patients, although that is much more modest and the 5 year survival rate for this class hovers around 30%. Unfortunately, many patients appear to be intrinsically resistant to these therapies and gain no benefit at all, and most others acquire resistance with time, forcing the field to reckon what is next in the post CDK4/6 inhibitor space? While there have been advances in developing drugs that can adjust hormone levels, they haven’t led to significant improvements in how long people live with the disease. As a result, there’s still a need for new therapies that can make a bigger difference in improving survival rates.
But the field is responding and several new medicines have entered clinical usage in the last few years, with the goal of providing additional choices to delay the use of chemotherapy and increase overall survival.
The consensus now is that these CDK4/6 inhibitor resistant breast cancer patients should be screened for several genetic perturbations, which are now actionable in terms of novel therapies. Olaparib, capivasertib or everolimus are all new additions to the post CDK4/6 inhibitor arsenal. This use of precision oncology screening in the breast cancer space reinforces the observation that not all metastatic disease is the same and this heterogeneity requires understanding on a per-patient level and therapies may have to be administered sequentially as disease evolves. Even when a patient needs to move to chemotherapy, for many, a less toxic option may now be available. Enhertu is an antibody drug conjugate (ADC), or a chemotherapy linked to an antibody that recognizes the Her2 receptor.
This therapy was approved with great fanfare as it helps target the chemotherapy to the Her2+ tumor cell and has been shown to reduce toxicity relative to the untethered chemotherapy. Many CDK4/6 inhibitor resistant patients have now been reclassified as eligible for this therapy with the advent of a new biomarker designation, Her2 low.
Of course, all of these new therapies carry potential adverse effects with them, and that is part of the reason for the robust pipeline of new therapies in the phase one clinical trial or preclinical setting. The clinical resistance seen with the CDK4/6 inhibitors appears to be due at least in part to the activation of a previously undrugged target, CDK2. While the field has tried unsuccessfully for several decades to drug CDK2, new more specific CDK2 monotherapies have entered phase one (Ph1a) trials over the last year (Pfizer, Blueprint Medicine, Incyclix, Incyte). The CDK2 monotherapies may have more limited response due to observations that both CDK4/6 and CDK2 have to be inhibited simultaneously, so there is effort to combine them with either existing CDK4/6 inhibitors such as Ibrance or new, more untested CDK4 inhibitors: Pfizer is testing a new CDK2 and CDK4 inhibitor combination and Beigene will begin testing of their new monotherapy combinations.
The incredible focus in the drug-resistant breast cancer space will likely drive the development of therapies that will ultimately cross over into usage in other tumor types. For example, the Destiny trial last year demonstrated that Enhertu, which was originally developed for and approved in a different form of breast cancer, Her+ BC, showed response in numerous other tumor types, including uterus, cervix, ovaries, bladder, which were Her2+ paving a way for its broader use. A second observation is the sequencing of these new therapies combined with biomarker analysis, or identifying additional actionable targets in each patient, will be important to continually add to the therapeutic pipeline for patients. Creating a repertoire of add-on possibilities should help reduce the stigma of metastatic breast cancer as a terminal disease.
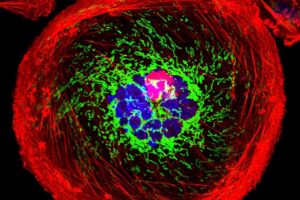
Public domain image by the National Cancer Institute
Dr. Blain is an internationally known expert in cell cycle and cancer biology, and is one of the world’s experts on p27Kip1. She has been studying cell cycle regulation for more than 25 years as an NIH funded investigator and tenured Associate Professor at the SUNY Downstate Medical Center. She founded Concarlo Therapeutics, capitalizing on discoveries she made and patented. She was trained at Princeton, Columbia and the Memorial Sloan-Kettering Cancer Center.














