
The established environmentalism mantra of “reduce, re-use, recycle” opened the door for medical device manufacturers to roll out recycling programs under the guise of sustainability efforts. But, in practice, these programs aren’t benefiting anyone except the manufacturers themselves. Hospitals would be much better served by focusing on reuse and reprocessing programs instead, but in many cases, their hands are tied.
Let’s examine why this is the case — and why this needs to change.
The unsustainable costs of device recycling

The Funding Model for Cancer Innovation is Broken — We Can Fix It
Closing cancer health equity gaps require medical breakthroughs made possible by new funding approaches.
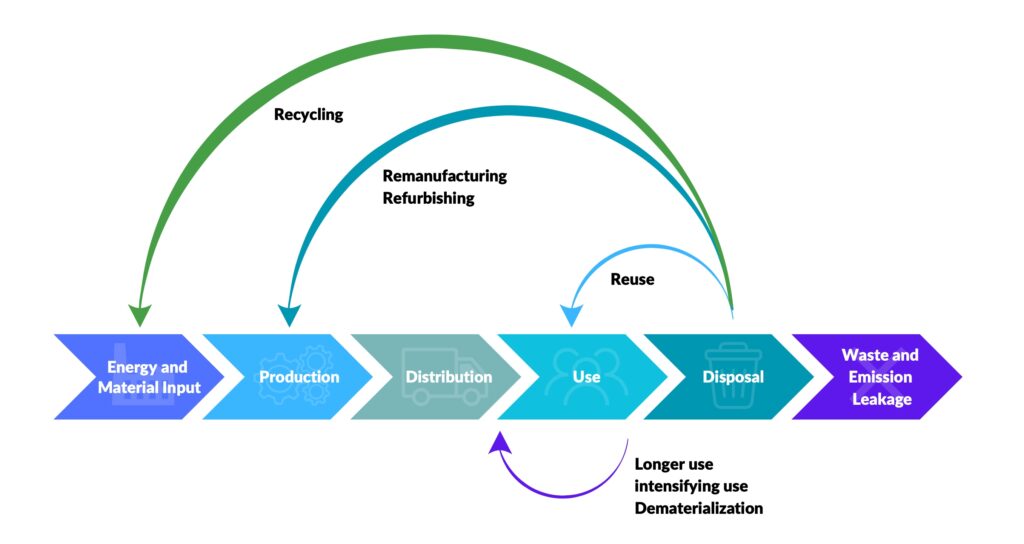
When it comes to medical devices, there are multiple concepts being employed in the name of sustainability, including:
- Reuse: Reusable devices are designed by the manufacturer to be re-used a specified number of times.
- Reprocessing: Reprocessing is a process through which FDA provides clearances to reprocessors to collect, identify, clean, test, and sterilize used single-use medical devices and sell them back to the hospital.
- Recycling: With recycling, devices are broken down to their component parts, and some materials (but not all) are recycled.
Recycling of medical devices is the most “expensive” sustainability solution for at least three reasons:
- Environmental: When a device is recycled, some materials (but not all) are recycled. (The industry has suggested that about 23 percent of surgical waste can be recycled. Many parts of a typical cardiology device, for example, simply cannot be recycled.) This process involves a lot of energy consumption. Comparatively, reprocessed devices are a more environmentally friendly option and have less than half the environmental impact of a new device in terms of carbon emissions.
- Financial: With recycling, the hospital still has to purchase a new device. Comparatively, hospitals can buy reprocessed devices back at a fraction of the cost of a new device.
- Supply chain: When used devices are broken down to their component parts and recycled, these devices are taken out of the supply chain. At a time when hospitals experience backorders on some of their most critical devices, recycling seriously threatens supply chain resilience.
Legacy sustainability programs in healthcare were straight-forward recycling programs — and very expensive initiatives. On the other hand, today’s emerging circular programs — which focus more heavily on reuse, repair, and reprocessing — combine environmental sustainability with financial upside. When an item is not broken down into its component parts, but rather made ready for a second use, there is balance in the sustainability-cost equation. Truly circular solutions reduce costs and environmental impact.
(image provided by the author)
Physicians as environmental sustainability champions in healthcare
So, how should hospital supply chains use this information? Single-use devices are bad for the environment and for hospital economics. Reusable devices represent the most environmentally responsible solution. When single-use devices are all that is available, reprocessable devices should be preferred. Recycling solutions are the least valuable option from both an environmental and a financial perspective.
Notably, physicians are becoming more committed to responsible environmental solutions as it relates to their device use. As an example, a recent study found that electrophysiologists are highly motivated to reduce the environmental impact of electrophysiology procedures. A total of 278 physicians from 42 hospitals were polled, and 62 percent were motivated to work toward more sustainable solutions. The re-use of catheters was the most commonly cited potential sustainability solution by the respondents.
This is great news in labs where more than half of catheters used are discarded to medical waste, and less than 20 percent of catheters are re-used. There are two ways to increase re-use in the EP lab: Manufacturers can design and market reusable catheters instead of single-use catheters, or hospitals can work with reprocessing companies to use reprocessed single-use catheters.
The manufacturer’s role in perpetuating unsustainable programs
So, how are manufacturers responding to this desire from physicians to become more sustainable? We have seen some of the largest manufacturers start “sustainability programs” based on recycling of medical devices. It seems like they are responding to an increased demand for environmental sustainability in the hospital. However, the problem is that these types of programs just are not as good as they sound. In fact, they work counter to the intention and further exacerbate some rather serious problems in the supply chain. They do, however, ensure that the manufacturers can continue to grow their revenue.
From an environmental perspective, as noted above, recycling is a far less valuable circular solution than reprocessing. Devices from these programs will not be re-used, but rather broken apart, and the recyclable parts (less than 30 percent of residual hospital waste) will be used in the manufacture of other products. If, instead, the devices were reprocessed, the entire catheter would be salvaged and made available for another use with the use of very few resources.
Since many single-use devices can be reprocessed and re-used, putting in place a recycling program simply means that the environmental benefit is lessened. A recycling program that implies that a new catheter will be needed. In other words: Every time a catheter is recycled rather than reprocessed, the hospital increases CO2 emissions significantly.
So why would some of the largest suppliers of medical devices put a program in place that increases CO2 emissions and makes supplies scarce? It’s a simple matter of math: Every time a medical device is recycled rather than reprocessed, the manufacturer increases its revenue while the hospital increases its costs. This is because the hospital cannot buy a reprocessed medical device at the lower price but must buy a new one. Possible supply shortages, environmental harm, and hospital economics are collateral damage.
This is the only way medical device recycling programs make sense: when they make sense (and cents) for the manufacturer. Meanwhile, the environment, the hospital, and the patients must pay the price. It’s time for this narrative to change.
Photo: ChrisGorgio, Getty Images
Lars Thording, PhD, serves as vice president of marketing and public affairs at Innovative Health LLC. He has a background in academia, consulting, and industry leadership. He has been responsible for the launch of numerous market-disrupting solutions across healthcare, insurance, and technology. Originally from Denmark, Thording has taught at universities in Denmark, Ireland, and the United States. He currently serves as the vice president of marketing and public affairs at Innovative Health, a medical device reprocessing company specializing in electrophysiology and cardiology technology. Lars currently serves on the board of the Association of Medical Device Reprocessors.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.










