A pharmaceutical ingredient that’s been a key component in nasal decongestants for decades is having its efficacy called into question, and the FDA is now weighing whether to change the compound’s regulatory status — potentially leading to many widely used over-the-counter cold and allergy products being pulled from pharmacy shelves. But before the FDA takes any action, it wants to hear what the public thinks.
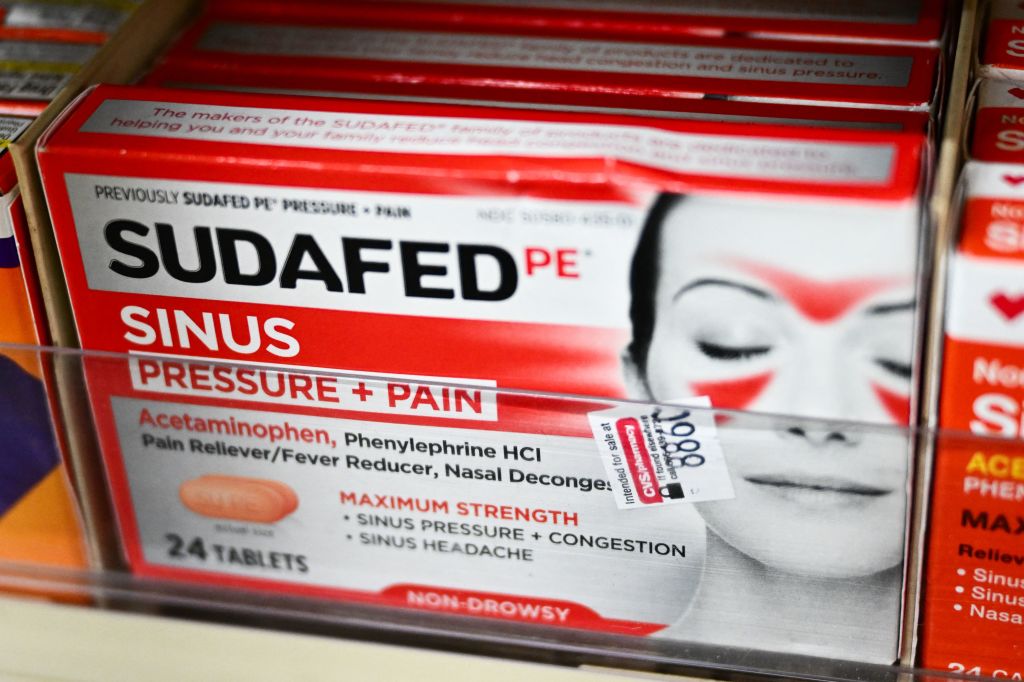
The ingredient, oral phenylephrine, by itself and in combination with other active ingredients, is in decongestants sold under numerous brand names, such as Sudafed and Mucinex. All products containing oral phenylephrine continue to be available to consumers for now. But on Thursday, the FDA proposed an order that would remove oral phenylephrine from its non-prescription drugs guidelines, called the OTC Monograph. The regulator emphasized that this proposed order is due to lack of efficacy, not because of safety.
At one time, phenylephrine was rare in decongestants because pseudoephedrine was the preferred active ingredient. But that compound can be made into methamphetamine. Efforts to curb meth production led to the Combat Methamphetamine Act of 2005, which moved pseudoephedrine-containing drugs behind pharmacy counters. Drugmakers responded by making more products with oral phenylephrine, which is not covered by this law.
Last year, an FDA advisory committee discussed phenylephrine and unanimously voted that current scientific data do not support the ingredient’s efficacy as a nasal decongestant. The committee raised no concerns about the safety of oral phenylephrine when used at the recommended dose. The FDA now says it has conducted a comprehensive review of all available safety and efficacy data for oral phenylephrine as a nasal decongestant, including historical data used to support the compound 30 years ago. Speaking during a conference call with journalists Thursday, Theresa Michele, director of the FDA’s office of nonprescription drugs, said new data had become available since the advisory committee meeting, which the agency also reviewed.
“At this point, based on the available data, and taking into account the advice of the advisory committee, we are proposing that oral phenylephrine is not effective to relieve nasal congestion at the recommended dose set forth in the monograph,” Michele said.
Phenylephrine is also an ingredient in some nasal spray decongestants. The FDA’s proposal does not extend to such products. The proposed FDA order can be found here. Public comments may be submitted here (use docket number FDA-2024-N-4734 ) through May 7, 2025. After considering the comments, the agency may issue a final order removing oral phenylephrine from its guidelines, which would mean nasal decongestants could no longer contain the compound. Michele said the FDA would then provide manufacturers with time to either reformulate their medicines or remove oral phenylephrine-containing products from the market.
Don’t let the autumn sniffles get you down. Here’s a look back at other recent regulatory news, including U.S. and European actions on several novel medications (alas, no new decongestants):
Decisions for Drugs and Devices
—The FDA needs more time to review Organon drug Vtama as a treatment for atopic dermatitis. The company said the regulator has pushed out the December target date for a decision by three months to March 12, 2025. Vtama is from Roivant Sciences subsidiary Dermavant, which Organon recently acquired for $175 million up front. Under Dermavant, the topical drug won FDA approval in 2022 as a treatment for plaque psoriasis.
—Novartis cancer drug Scemblix expanded its FDA-approved uses to include the treatment of newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia (Ph+ PML). The tablet, part of a class of drugs called STAMP inhibitors, initially landed accelerated FDA approval in 2021 as a treatment for advanced cases of Ph+ PML.
—The FDA approved Iterum Therapeutics antibiotic Orlynvah. The regulatory decision covers the treatment of uncomplicated urinary tract infections in women who have limited or no oral antibacterial treatment options. The drug, whose main ingredient is sulopenem, is taken as a tablet twice daily for five days.
—Astellas Pharma landed FDA approval for zolbetuximab, brand name Vyloy, as a treatment for gastric or gastroesophageal junction adenocarcinoma. It’s the first FDA approval for a drug targeting the cancer protein claudin 18.2 (CLDN18.2). The regulatory decision specifically covers patients whose cancer is negative for a different cancer protein called HER2. Drugs are already available for HER2-positive cancers.
—In other Astellas news, the Japanese pharma company withdrew its European Medicines Agency application for geographic atrophy drug avacincaptad pegol. The company said it made the decision after discussions with the agency’s Committee for Medicinal Products for Human Use. The drug, administered as a once-monthly eye injection, won FDA approval in geographic atrophy last year and is marketed in the U.S. under the brand name Izervay. Failure to secure approval in Europe will make it harder for Astellas to recoup the $5.9 billion it spent to acquire Iveric Bio, the company that developed the drug.
—Pfizer respiratory syncytial virus vaccine Abrysvo expanded its FDA approval to include adults age 18 through 59, broadening the market for the product. The initial FDA approval of Abrysvo last year covered patients age 60 and older. It’s also approved for use by pregnant individuals as a maternal vaccine; antibodies produced by the mother confer protection against RSV intended to last from the baby’s birth up to six months of age.
—Gilead Sciences’ Trodelvy will no longer be available in the U.S. for treating urothelial carcinoma, an aggressive bladder cancer. After discussions with the FDA, the company decided to voluntarily withdraw the product, which had won accelerated approval in this indication in 2021. In May, the company reported Trodelvy failed its confirmatory Phase 3 test in advanced urothelial carcinoma. The withdrawal in urothelial carcinoma does not affect drug’s approved uses in breast cancer.
—After previous regulatory setbacks, AbbVie finally landed FDA approval for Vyalev, a Parkinson’s disease drug/device combination product that provides 24 hour subcutaneous infusion of the medications foscarbidopa and foslevodopa. Last year, the regulator turned down the product’s application, asking for more information about the pump in the device. The FDA did not raise any questions about safety or efficacy, nor did it ask for another clinical trial. This past June, the agency again turned down AbbVie’s application for issues at the product’s third-party manufacturer.
—There’s a new Pfizer drug for both hemophilia A and B. The FDA approved the antibody drug marstacimab for preventing or reducing frequency of bleeding episodes in patients 12 and older. Pfizer will market the drug under the brand name Hympavzi. As a once-weekly injectable medication, Hympavzi will provide an alternative to IV-infused hemophilia therapies.
—The FDA needs more time to review Intercept Pharmaceuticals’ application seeking full regulatory approval of Ocaliva, which had received accelerated approval in 2016 for the rare liver disease primary biliary cholangitis. Intercept, now a subsidiary of Alfasigma, said the agency did not provide a new date for a regulatory decision.
—Alzheimer’s disease drug Leqembi hit a regulatory obstacle in Australia, where the Therapeutic Goods Administration decided against registering the medication. Eisai said it will request a reconsideration as permitted under Australian law. It’s the second setback for the drug in recent months. Over the summer, the drug received a negative opinion from a European Medicines Agency committee concerned about the risk of severe side effects and limited benefit. Leqembi has approvals in the U.S., Japan, China, and several other markets.
—The FDA approved a Thermo Fisher Scientific companion diagnostic to Voranigo, a Servier Pharmaceuticals’ drug approved over the summer for treating patients whose glioma is driven by mutations to IDH1 or IDH2 enzymes. The diagnostic, called Ion Torrent Oncomine Dx Target Test, identifies patients whose cancer carries the genetic signature making them eligible for treatment with the Servier drug.
—Advanced cases of non-small cell lung cancer can now be treated with a wearable device. The FDA approved Novocure’s Optune Lua, a wearable technology that kills cancer cells with electrical signals administered via electrodes placed on the skin. Novocure’s “tumor-treating field” technology was first approved in 2011 as a treatment for a recurrent type of brain cancer.
—The FDA rejected Zealand Pharma’s dasiglucagon, a drug developed to prevent and treat hypoglycemia in children who have the rare disease congenital hyperinsulinism. According to the Copenhagen-based biotech, the regulator cited issues at a third-party manufacturer. The FDA did not raise any concerns about the drug’s clinical data or safety.
Advisory Committee Outcomes
—An FDA advisory committee voted 11 to 3 that the benefits of Lexicon Pharmaceuticals’ sotagliflozin do not outweigh its risks when used as an adjunct to insulin to treat adults with type 1 diabetes and chronic kidney disease. But some committee members expressed support for use of the drug in subpopulations of patients. Sotagliflozin, given the brand name Zynquista, is expected to receive an FDA decision by Dec. 20. Sotagliflozin was approved last year for the treatment of heart failure and is marketed as Inpefa in this indication.
—The European Medicine Agency’s Committee for Medicinal Products for Human Use yet again recommended against renewing the marketing authorization for Translarna, a PTC Therapeutics drug for Duchenne muscular dystrophy. Translarna received conditional marketing authorization in 2014. After the drug failed its Phase 3 study, the committee twice recommended against renewing the authorization. The latest opinion comes after the EMA directed the committee to reconsider, taking into account “the totality of evidence.” The committee said its reassessment “concluded that the effectiveness of Translarna has not been confirmed.”
—Stealth BioTherapeutics moved a step closer to potential approval of the first drug for Barth syndrome. An FDA advisory committee voted 10 to 6 that Stealth’s drug, elamipretide, was effective at treating the ultra-rare mitochondrial disorder. The committee vote follows several regulatory setbacks, including a 2021 refuse-to-file letter in which the FDA pointed out that elamipretide failed its clinical trial. Stealth maintains there was improvement in a subgroup of patients and the short duration of treatment is the reason for the trial failure. An FDA decision is expected by Jan. 29.
What’s New in Covid-19
—The European Commission granted marketing authorization to Novavax’s updated Covid-19 vaccine, Nuvaxovid. Authorization for the protein-based vaccine covers its use in those age 12 and older. The FDA authorized the updated version of Novavax’s Covid-19 vaccine in September.
—In other Novavax Covid-19 news, the FDA pressed pause on the company’s plans for late-stage testing of a combination flu/Covid-19 vaccine as well as a standalone influenza vaccine. According to Novavax, the clinical hold stems from a report of motor neuropathy in a single patient outside the U.S. who received the combination vaccine in a Phase 2 study. The trial was completed in July 2023 and the serious adverse event was reported in September. Novavax said previous Covid-19 and influenza trials showed no signs of motor neuropathy. The company’s standalone Covid-19 vaccine is unaffected by the clinical hold.
—In Covid-19 and flu testing news, the FDA granted marketing authorization to a Healgen Scientific over-the-counter, at-home test for both pathogens. The OTC Healgen Rapid Check Covid-19/Flu A&B Antigen Test uses a sample from a nasal swab. The authorization covers use of the product by people age 14 and older within five days of the start of symptoms. For children as young as 2, the sample must be collected by an adult.
Photo: Patrick T. Fallon/AFP, via Getty Images










