
With mandatory Alternative Payment Model Performance Pathway (APP) Reporting beginning in Performance Year 2025, the time to act is now. Reporting quality on all beneficiaries marks a major shift, requiring thoughtful preparation and strategic planning. If your Accountable Care Organization (ACO) hasn’t started yet, don’t worry — there’s still time to get on track.
The first essential step: finalize your plan by determining your optimal reporting method.
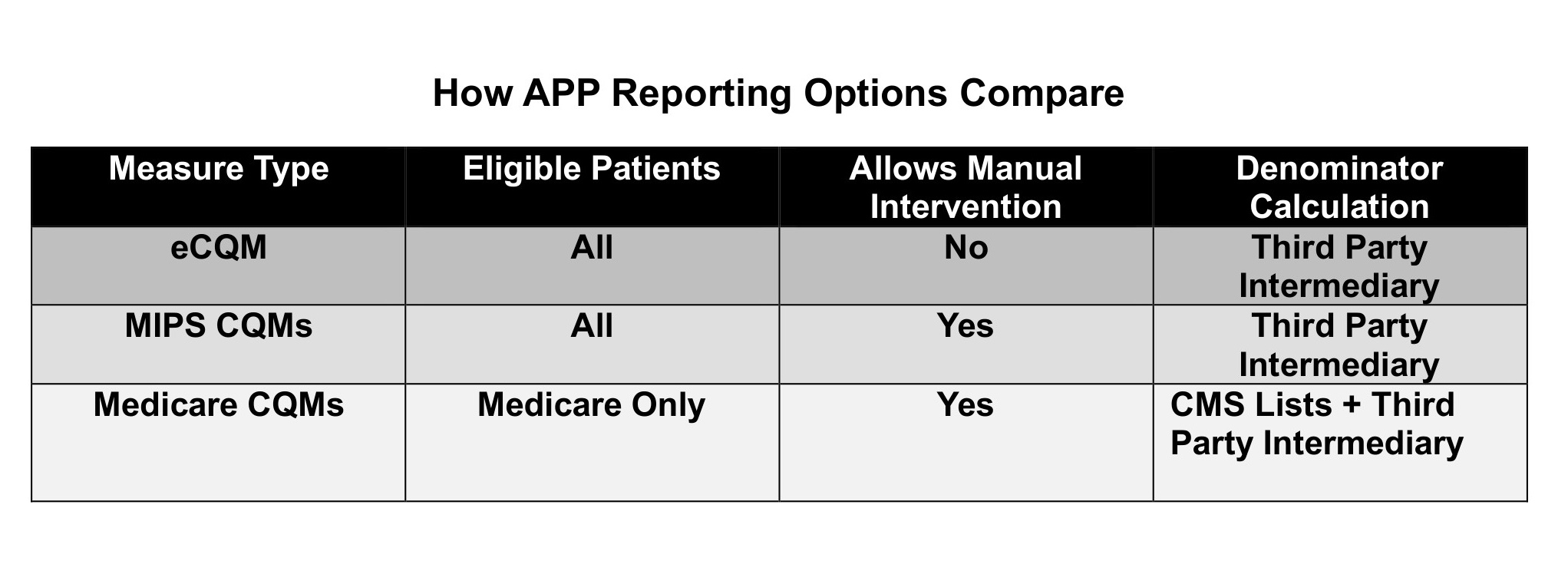
Not sure of the best method for your ACO to perform APP Reporting? You have three reporting options — Electronic Clinical Quality Measures (eCQMs), Merit-based Incentive Payment System Clinical Quality Measures (MIPS CQMs), and Medicare Clinical Quality Measures (Medicare CQMs). Here are the differences between these approaches, and why the decision regarding “best method” is not automatic. It will depend on your participating physician practices, their Electronic Health Records (EHRs), and your desire for data.
How APP Reporting Options Compare
Knowing whether you have the ability to perform eCQM Reporting is an essential first strategy.
Why? Many organizations want to use this approach because one electronic source document, a QRDA-I, captures both denominator and numerator of measures. If your system can do it, it’s easy for the organization (but probably the most expensive method). If you can’t meet the conditions, you will need to perform APP Reporting through either MIPS CQMs or Medicare CQMs. Let’s examine the eCQM question first, because it is the most basic.
eCQMs: Issues for APP reporting
eCQMs have a number of issues in APP Reporting because they require a standardized data source, called the QRDA-I, which certified EHRs use as a quality reporting tool to capture and report measures. To use eCQMs in APP Reporting, you need to meet two conditions that are challenges for multi-EHR ACOs:
- Each individual practice EHR must be able to generate a QRDA-I, the data format required for eCQM reporting. If you have practices with systems that are not ONC-Certified, or if even one practice has no EHR, you will not be able to meet this condition. Even some certified EHRs are not able to export a QRDA-I outside the system. To be certain that you can meet this condition, you will need to test each practice EHR to validate that you can produce patient data in a QRDA-I from every practice.
- Patient data from QRDA-I files across all systems must be aggregated and patients must be de-duplicated through patient matching and integration of data. APP Reporting requires that patients are uniquely reported only once, with the latest measure value. This will require technical work from your Qualified Registry vendor, if you have more than one EHR.
Are there similar conditions for MIPS or Medicare CQMs? Not exactly. CQMs can be reported using any kind of data format that can be validated by the patient’s clinical record. But each has advantages and disadvantages.
MIPS CQMs: Higher flexibility, potentially higher cost and reporting burden
MIPS CQMs was a preferred choice of many ACOs, especially those with many systems, because of flexibility in data source formats for both numerators and denominators. Your ACO can aggregate QRDA-Is, flat files, and any external data to use in APP Reporting, as long as it is backed by the clinical record. That data is of high value for many other ACO purposes, such as population health, cost management, analytics, and health equity. EHRs must be able to produce reports from their systems, which most can do. This will initially involve ACO or practice staff to generate data files, and require intermittent involvement thereafter.
Medicare CQMs: Data aggregation still required, highest reporting burden for most ACOs
The Medicare CQM option is based on the desire to limit ACO workload in data aggregation. But the Centers for Medicare & Medicaid Services (CMS) has modified its guidance here. While CMS will be providing quarterly lists of patients who are eligible for measures based on claims, these aren’t enough. ACOs must validate eligibility with their own data, which means that ACOs will still need to aggregate data from practice management systems to verify patient coverage, visits, and diagnoses.
Like MIPS CQMs, Medicare CQMs have more flexible data sources for gathering clinical (numerator) data. But for ACOs seeking to lower their costs and depending on manually looking up and submitting values, this reporting method comes with a much higher staff burden.
Your decision criteria
Your ACO should investigate which method will create the most accurate, complete reporting involving the least work for your organization. If you are a large organization with one or two big systems, you will most likely be able to produce QRDA-Is or FHIR files to fulfill the requirements. If you are a smaller organization with multiple systems, you need to test your practice systems’ results first.
If your ACO has been struggling to decide which method is “superior” for APP Reporting, we can assure you that any of these methods can produce true and accurate results. Which is optimal, on the other hand, will depend on your ACO limits and goals:
- If cost is your biggest concern, use Medicare CQMs — but understand that, depending on your patient count, it might require staff work. As the number of measures grows, so will the work.
- If your long-range goal is driving outcomes and health equity, your solution will eventually need more data. You can start with Medicare CQMs, but plan to use eCQMs or MIPS CQMs for the following year.
Remember that the ultimate CMS plan is to require more measures and (interoperable) digital measures, which will build toward a more robust data solution in the future. Taking steps now is the best way to get started for long-term reporting solutions.
Photo: Witthaya Prasongsin, Getty Images
Theresa (Terry) Hush is a health care strategist and change expert with experience across the health care spectrum. Terry’s broad range of health care experience includes executive positions in public, non-profit and private sectors, from both payer and provider sides of the business, peppered with health care public policy and regulation experience. She is co-founder and CEO of Roji Health Intelligence, formed in 2002 to help providers implement Value-Based Care with technology and data-guided services. An expert at creating consensus for desired change through education and collaboration, Terry helps organizations to move toward cost and outcome accountability to achieve growth.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.











