Given the remarkable advances seen with gene therapies for sickle cell disease (SCD), it may seem counterintuitive to suggest the space may be in need of more therapies that have already been established. Indeed, as cutting-edge therapies face a long journey to treat patients at scale, the community recently faced a setback with the withdrawal of one of the few previously approved drugs over safety concerns. Drug-based therapy, starting with hydroxyurea, has been the first line course of treatment for patients with SCD. But the approved drugs are not uniformly accessible globally, nor are they effective for every patient, and many are concerned about their side effect profiles.
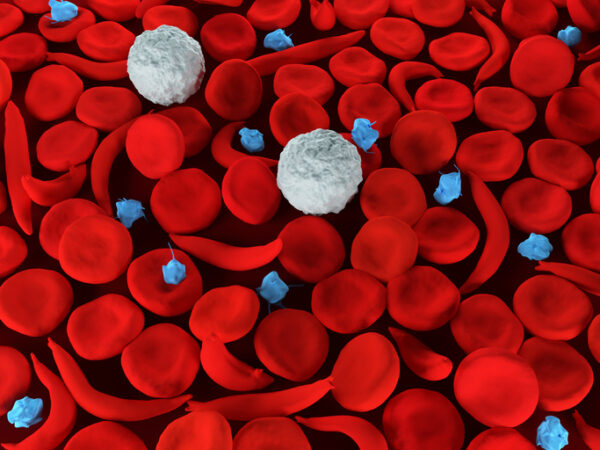
Iterations of the first therapies for SCD still have disease-modifying effect and the potential for broader use, especially for patients who don’t respond to drug therapies. In the 1960’s, shortly after the disease’s molecular mechanisms were first understood, blood transfusion therapy became commonplace to treat complications from SCD.
Today, blood-based therapies are safe, effective – and underutilized, with access limited even in developed regions. Until we reach the day where curative gene therapies are affordable and globally available, we must shake off the paradigm of drug-only SCD treatment to improve the lives of patients everywhere.

Improving the Healthcare Financial Experience to Help Care Flow
Zelis CEO Amanda Eisel shares her perspective on how the company is solving the problems of a fragmented health financial system to benefit all.
Blood therapy advances
Without a doubt, hydroxyurea (and other pharmaceuticals) saves lives and reduces the suffering for a significant proportion of patients. However, it is not universally accessible, and medications alone are not always sufficient to prevent acute pain crises or life-threatening SCD complications. The market withdrawals of two drugs last year highlight the urgent need for alternative, scalable solutions that address unmet medical needs.
Even in this context, blood therapies are often overlooked. But many, like the World Health Organization, view blood therapy as a crucial treatment paradigm, and numerous advances over the past 60 years have made these approaches more attractive for many disease areas, particularly SCD. One has been the move beyond simple transfusion to red blood cell exchanges (RBCX). If a patient receives too many transfusions, there is risk for a complication known as iron overload. RBCX addresses this by removing the blood cells that have abnormal hemoglobin proteins and replacing them with healthy donor material.
Further, RBCX today can be automated, which shortens the procedure and increases the time between them. Automated RBCX has been shown to reduce hospitalizations due to pain crises, improve recovery from a dangerous respiratory complication known as acute chest syndrome (ACS), and prevent strokes. Besides clinical improvements, a recent meta-analysis of 20 years’ worth of data showed patients often see quality-of-life improvements including reduced pain, fewer hospitalizations and procedures, and fewer complications. This contributes to improved social functioning and lower anxiety as well.
Improving access
Regional differences translate to significant disparities in all SCD treatments, including and especially automated RBCX. Healthcare systems with more resources tend to enable better access, and there are visible efforts to improve further. In February 2024, for example, UK’s National Health Service invested £1.5 million ($1.9 million) to make automated RBCX available more broadly, with the potential to enable 10,000 more procedures annually.
In the U.S., automated RBCX usually takes place in a hospital, limiting blood therapy access for people with SCD in rural areas. In 2023, Center for Medicare and Medicaid Services (CMS) adjusted rates so that community healthcare facilities are reimbursed more on par with hospitals, which may encourage an increase in procedures done closer to where patients actually live.
SCD is a genetic disease inherited by people with African ancestry, and the vast majority of patients globally fall outside the UK and U.S., where automated RBCX is most common. In Latin America and Middle Africa, access to even basic treatment for SCD is limited. Our experiences in the U.S. and UK can be a starting point for countries with high SCD prevalence, which will need to build infrastructure, including access to enough safe blood, and collect the relevant data to support guidelines for standards of care.
In addition, improving quality of life in the global SCD community will take significant investment and collaboration across the patient pathway, and increased access to automated RBCX will play an important role.
New approaches
The focus on medicines as a panacea in SCD has reinforced standards of care that underutilize blood therapies. Thankfully, the landscape is beginning to change.
In 2023, as part of an effort to define global therapeutic strategies, a Lancet Haematology Commission identified long-term RBCX as a consensus therapeutic approach for atypical pulmonary hypertension and stroke prevention, and standard intervention for acute organ damage and recurrent ACS and pain crises.
And last year, an international panel of multidisciplinary experts published recommendations for SCD prenatal care. Among other guidance intended to be adapted based on available resources, the new recommendations outlined when patients are likely to benefit from automated RBCX.
More studies are also in progress, including one that will inform the use of automated RBCX as part of the standard of care for patients suffering from ACS.
Government intervention is also key. Brazil’s public healthcare system recently included RBCX as a second-line treatment to help prevent the complications associated with SCD like stroke. The Indian government has embarked on a targeted mass screening initiative that aims to improve early diagnosis and build awareness as it aims to completely manage and prevent the disease by 2047. And in Kenya, SCD patients will now receive enhanced healthcare coverage, including RBCX, under the new Social Health Insurance Fund (SHIF).
Further partnership is needed, involving all stakeholders – healthcare providers, patient advocates, government and non-profit groups, as well as therapeutics and technology companies. In some regions where SCD is prevalent, major changes are needed to blood systems to increase donations and improve safety. The World Coalition on Sickle Cell Disease, launched in 2023, is an excellent example of the type of collaboration that will be needed to expand access to blood therapies and other critical treatments.
The patient journey
RBCX is already an important part of the SCD therapeutic continuum, but we still lack a commitment to increase access across all regions. This long-term investment is crucial because automated RBCX is expected to remain a part of the patient journey for the therapies of the future. The procedure is used as a necessary part of the pre-treatment conditioning in preparation for curative gene therapy treatments and hematopoietic stem cell transplants.
In the meantime, patients with SCD clearly benefit from having various kinds of disease-modifying treatment options, with blood-based alternatives or adjuncts for drug-based treatment. Blood therapies remain a necessary and well-established part of any effort to improve the wellbeing and quality of life for a patient population that has been underserved for too long.
Image by Meletios Verras, Getty Images
Koenraad Dierick is the Vice President Patient Access at Terumo Blood and Cell Technologies. He leads a global team of government affairs, medical affairs and market access experts focused on interacting across the healthcare environment to remove barriers that prevent patients from accessing the care they need. Using evidence generation, medical education, awareness building and health economics his team is responsible for ensuring the company’s technologies directly improve the health outcomes of patients through appropriate funding and evaluation in target global geographies, ultimately resulting in more patients gaining access to treatments. Koenraad has over 20 years of experience in business development, market access, government affairs, medical education and market research across different industries including medical devices, pharma, life sciences, cell therapy, OTC, and fast-moving consumer goods.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.











