Oral health has an image problem. It’s often dismissed as an afterthought, inconvenience, or cosmetic procedure, a noticeable difference to how we prevent heart disease with wide-scale public awareness campaigns and robust early detection programs.
Why this disparity? It’s partly because heart disease can lead to immediate and sometimes fatal outcomes with heart attacks and strokes. Meanwhile, oral health issues like cavities and gum disease tend to develop more slowly, making it harder for people to know when an inconvenience is life-threatening.
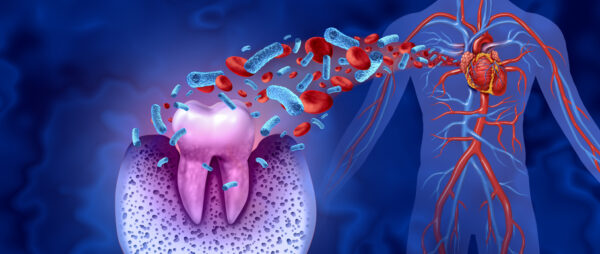
Because dental diseases tend to gradually worsen over time, there’s a common misperception that they are not serious or just a source of discomfort. But oral infections are associated with serious health issues like heart disease, diabetes complications, or other brain infections. This leaves out the hidden costs of dental diseases, like ER visits, school absences, and lost productivity, which can cost the US more than $45 billion and result in children losing 34 million school hours annually.
It’s time we treat dental care with the same urgency as other chronic disease prevention programs. Routine preventive care isn’t just good medicine; it’s smart policy. Here’s how we start.
Expand preventative dental coverage
Only 73% of adults in the US have dental coverage, significantly lower than the rates for health insurance. Plus, out-of-pocket costs constitute a significant portion of dental spending, often exceeding the share of out-of-pocket expenses in healthcare: in 2024, out-of-pocket costs accounted for 40.3% of total dental expenditure, significantly higher than the 10.6% out-of-pocket share of total health spending.
One driving factor is that most Medicare plans exclude dental coverage. In 2019, nearly 24 million people, or about half of all Medicare beneficiaries (47%), did not have any form of dental coverage, and while there is no newer data available, there is no sign that this number has decreased. While some people are able to gain dental coverage through Medicare Advantage, that alone is not enough, since those benefits tend to be more limited.
Without dental insurance, adults are more than twice as likely to report being unable to afford dental care. This leads to higher rates of severe tooth loss (8.5%), severe periodontitis (14.3%), and untreated caries (37.9%) among those unable to afford care.
A lack of preventive care also results in more emergency room visits for dental issues. An estimated 11% of avoidable ER visits from 2005 to 2016 were for dental problems, which could have been managed with regular dental care.
Expanding preventative dental coverage can encourage more people to receive routine checks and reduce some of the most common barriers to coverage. But to drive home the importance of routine dental care, we must invest in public health education campaigns to help people understand what’s at stake.
Invest in public education initiatives
Most people view routine dental checkups as “just a cleaning” when they are a critical screening for a potential chronic illness, just like any other health exam. Adding to this challenge is the misperception that people only need to see a dentist about an issue if they feel pain or discomfort. Early intervention is a fundamental principle in healthcare that applies universally — whether treating cancer or addressing dental disease, timely diagnosis and treatment are critical to success.
Research shows that improved levels of health literacy lead people to report their oral health as better and improve patient-dental communication. If people can understand what is at stake, they are more motivated to maintain consistent patterns of dental care.
In the same way that healthcare providers offer cholesterol checks, blood pressure screenings, and lifestyle counseling to reduce the risk of heart disease, we can make similar efforts by providing free dental screenings and public education.
We should also collect robust data to understand the value of these intervention efforts for improving oral health status and dental screening rates, similar to the data collection we conduct for cardiovascular risk factors. That way, researchers can understand barriers to coverage and how to best incentivize people to receive routine dental care.
Make over-the-counter oral care products FSA & HSA eligible
No example better illustrates the misunderstanding of the value of preventative dental care as FSA and HSA eligibility requirements. The IRS classifies dental items like floss and toothpaste as “general health products” rather than “medically necessary” items, putting them in the same bucket as items like shampoo. They are treated like an element of personal care rather than steps to address a direct medical need.
Thankfully, there is a bipartisan bill in Congress to make oral hygiene products FSA and HSA eligible: H.R.8599, the Oral Health Products Inclusion Act. Toothpaste, floss, and mouthwash all help prevent cavities and gum disease. To take oral health seriously, we cannot ignore the importance of reducing costs. Like nearly every other aspect of healthcare, preventative measures are the most effective way to reduce oral health issues, the overall cost of treatment, and loss of productivity.
Just as we’ve created comprehensive approaches to combat cardiovascular disease, implementing similar strategies for dental health would generate billions in savings while improving overall public health. But to even begin this process, we must view oral health as an essential component of our healthcare system, worthy of the same attention and resources we dedicate to other chronic conditions.
Photo: wildpixel, Getty Images
Dr. Teresa (Terri) Dolan is the Chief Dental Officer at Overjet, a dental AI platform. She is also professor and dean emeritus of the University of Florida College of Dentistry, where she served as dean and chief academic officer from 2003 until 2013. Dr. Dolan is a Phi Beta Kappa graduate of Rutgers University; she earned a DDS degree from the University of Texas and a MPH degree from the University of California, Los Angeles.
She was a Robert Wood Johnson Foundation Dental Health Services Research Scholar, completed a Veterans Administration Fellowship in Geriatric Dentistry, and is board certified in Dental Public Health. She currently serves as past-president of the Santa Fe Group, president of the American College of Dentists, and serves on the board of directors of the ADA Forsyth (formerly the American Dental Association Science and Research Institute).
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.











