A bitter irony defines the current American healthcare system. Patients have more urgent care and telemedicine options than ever before, but are increasingly turning to chatbots like ChatGPT. The front door to care is broken, and in response, patients are seeking answers wherever they can.
The problem:
Over 115 million “sick visits” overwhelm primary care offices each year, and the PCP shortage will continue to worsen in coming years. Meanwhile, one-third of Medicare 911 calls are for low-acuity issues that don’t require emergency care. Patients who face even one barrier to access are significantly more likely to end up in the emergency department over a year. The core problem is clear: the system is not matching the demand for healthcare services with the appropriate supply, and patients are often blamed for “abusing the emergency room.” This misses the real issue: most patients are not equipped to judge the urgency of their symptoms, especially when the average wait time for a primary care appointment exceeds three weeks in many areas.
Previous iterations of a “first-touch” solution to this problem include nurse advice lines and, more recently, automated symptom checkers. However, nurse lines may paradoxically increase emergency department visits and automated symptom checkers lack both diagnostic accuracy and contextual understanding. As a result, over 75 percent of patients bypass the formal healthcare system entirely, beginning their care journey with Google or, increasingly, ChatGPT.
The solution:
The growing use of AI chatbots for medical questions should not be seen as a threat to the healthcare system, but as a signal that patients aren’t trying to replace their physicians; they’re trying to find them. When someone types a medical question into ChatGPT, it’s a cry for help. Rather than dismissing this shift as misguided or unsafe, the healthcare system should interpret it as a wake-up call. We don’t just need more clinics or more apps; we need a reimagined front door to care.
The technology and infrastructure to support a new triage system already exists; we just haven’t connected the dots. The solution comes from combining scalable AI tools with clinical oversight to deliver smart, context-aware triage at scale. Imagine a patient describing their symptoms to a conversational AI interface that collects an initial history and notes potential red flags. That case is then asynchronously reviewed by a physician who has access to the patient’s health records and relevant data. In many cases, they’ll be able to direct the patient safely, whether to self-care, primary care, urgent care, or emergency care.

Transforming the OR: CEO Reveals Game-Changing AI Tech for Better Efficiency
How Apella leverages technology to increase OR efficiency.
Why it works:
This model doesn’t replace primary care, but redirects simple sick visits, helping patients navigate when and where a doctor’s office is the best next step. Essentially, this approach moves experienced physicians – scaled by AI – to the start of a healthcare journey, not the end. In emergency departments, this approach is known as “physician-in-triage”, and it improves outcomes and efficiency. In specialty care, electronic triage of consults have shown that a significant percentage of referrals, 32 percent in some GI settings and over half in dermatology, can be handled by primary care.
This is no longer just a vision; it’s timely and achievable. Regulatory shifts during the Covid-19 pandemic now enable reimbursement for asynchronous and audio-only telemedicine, allowing for innovative triage models. Federal rules under TEFCA and the 21st Century Cures Act are breaking down information silos, while generative AI enables accurate, low-cost history-taking. However, there are still some structural barriers that remain. The lack of national physician licensure complicates multi-state virtual care, reimbursement codes lag behind AI-assisted asynchronous models, and a culture of defensive medicine discourages appropriate care de-escalation.
But with proper support from policymakers, researchers, and technologists, these challenges are solvable. This is more than a tech opportunity; it’s a moral imperative. Decades of fragmented infrastructure have confused the patients it was meant to help, and now we must reimagine triage as the backbone of modern care: dynamic, AI-assisted, and physician-guided.
Photo: anyaberkut, Getty Images
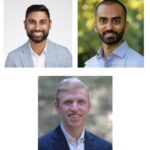
Dr. Rishi Khakhkhar is the Chief Medical Officer of Counsel Health, a physician-led, AI-native, asynchronous care platform. He is a practicing emergency physician and founding team member of Counsel Health. He leads their clinical team in building best-in-class asynchronous care models. In his previous role, he served as the medical director of Mount Sinai's Virtual Urgent Care, the largest telemedicine service in the health system. He also led emergency department operations for Hospital-at-Home and supported mobile integrated health efforts across the care continuum. He is deeply interested in patient-centric, tech-forward, and clinically sound approaches to improve healthcare access and affordability.
Dr. David Whitehead works on the Clinical Product team at Counsel Health, a physician-led, AI-native, asynchronous care platform. He is a practicing emergency physician who, at Counsel, is dedicated to developing innovative clinical tools that empower clinicians to deliver the highest quality asynchronous care. Prior to joining Counsel, Dr. Whitehead advised digital health start-ups helping set new standards in care delivery, assisting them in navigating clinical, operational, and strategic challenges. He also spearheaded the development of an asynchronous care program at Brigham and Women’s Hospital, focused on optimizing care transitions for patients after emergency department discharge.Dr. Whitehead is passionate about collaborating with mission-driven teams committed to enhancing healthcare accessibility and quality.
Dr. Muthu Alagappan is an AI researcher turned physician at the forefront of healthcare innovation. As the CEO and Founder of Counsel Health, he is pioneering a new paradigm in asynchronous, AI-powered healthcare, aiming to make high-quality medical advice accessible to all. Before founding Counsel, Muthu was the Chief Medical Officer of Notable Health and was an Attending Physician at Beth Israel Deaconess Medical Center and UCSF Medical Center. He graduated with his MD from Stanford Medical School, where he published several papers at the intersection of healthcare and AI. Currently, he practices at Counsel Health.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.