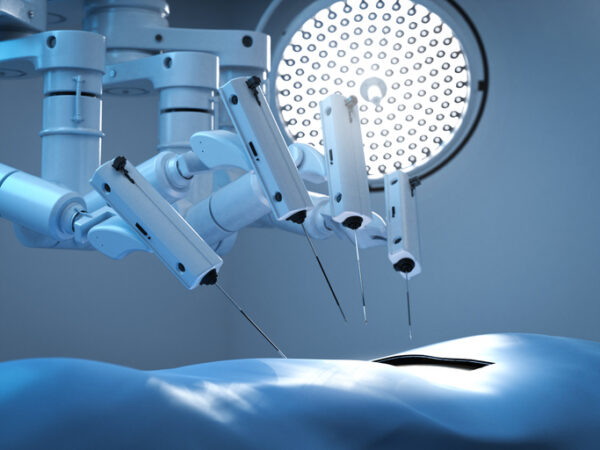
Over the past few years, rapid surgical robotics advancements in navigation, imaging, and workflow integration have transformed what’s possible in the operating room. As we look ahead to 2026, I expect that momentum to accelerate across three specific areas: new frontiers in imaging, the expansion of robotics into community hospitals, and the evolution of commercialization strategies.
Beyond anticipated advancements in technology, democratization of access marks a groundbreaking new phase for robotic surgery because it represents a shift in where these innovations are being adopted and who they can help. It means that within the next few years, revolutionary advances in access to minimally invasive surgeries will be easier at a much lower cost.
Robotic surgery reaches community hospitals
For years, surgical robotics was seen as the domain of large urban health systems and teaching hospitals. High capital costs, lengthy implementation timelines, and resource-intensive support models meant that only the largest institutions could adopt the technology at scale. That picture is changing.
In 2026, community hospitals will be an increasingly important growth engine for the field. Several forces are driving this shift:
- Patient access: Smaller hospitals want to offer the same minimally invasive procedures that attract patients to academic centers. Robotics helps them retain local patients who would otherwise travel for care.
- Economics: New business models, including subscription pricing, per-procedure economics, and more flexible service structures, are making robotics financially viable for hospitals with tighter budgets.
- Technological maturity: Platforms are easier to adopt, with faster installation, simplified workflows, and less reliance on large on-site support teams.
The result will be a broader patient population benefiting from robotic procedures. You can imagine patients in smaller urban areas or rural communities able to receive advanced care closer to home and their support networks. It also enables those providers to realize new revenue streams and allows hospitals of all sizes to participate in shaping the future of minimally invasive surgery.

The Power of One: Redefining Healthcare with an AI-Driven Unified Platform
In a landscape where complexity has long been the norm, the power of one lies not just in unification, but in intelligence and automation.
Imaging technologies step to the fore
Physicians’ ability to see inside the human body and accurately interact with anatomy continues to be a challenge. Even today, many older robotic platforms still rely on offline scans for navigating during procedures, which can lead to CT-to-body divergence.
Over the next year, I believe advances in real-time visualization, AI-powered reconstruction, and multi-modality fusion will continue to reshape how we see and interact with the body during procedures. I see three areas of particular importance:
- Higher-fidelity real-time visualization: New sensors and image processing techniques are enabling sharper resolution and greater depth of field, especially in flexible robotic scopes. This makes it possible to visualize smaller structures with greater clarity, reducing reliance on fluoroscopy and other adjunct imaging.
- AI-enhanced interpretation: Artificial intelligence is increasingly embedded directly at the point of care. These systems can highlight areas of interest, guide navigation, and compensate for suboptimal visualization in challenging anatomies. The most effective designs support, not replace, clinicians, acting as an additional layer of safety and precision.
- Cross-modality integration: One of the most exciting frontiers in imaging is combining streams like CT, ultrasound, and endoscopic video into a single, unified view. Robotic platforms are uniquely positioned to make this possible, offering a more comprehensive map of the procedure in real time.
In 2026, visualization will no longer be just about “seeing better” but instead about empowering clinicians with a deeper, data-rich understanding of anatomy, helping them make faster, safer, and more confident decisions in the procedure suite.
Commercialization gets more strategic
As technology evolves, so too do the ways we bring surgical robotics to market. For years, commercialization was dominated by large capital equipment models and long sales cycles. That model is being reimagined, and I expect 2026 to bring even greater changes.
This is because hospitals are increasingly looking for predictable, per-procedure economics rather than significant upfront investments. Disposable scopes and subscription-based service models align well with this trend, providing more flexibility for health systems facing tight budgets.
At the same time, the focus is shifting from volume to value. With healthcare economics under pressure worldwide, stakeholders are scrutinizing whether new technologies deliver measurable improvements in outcomes and efficiency. Evidence generation is becoming as important as engineering. Companies that can demonstrate real-world impact with shorter procedures, fewer complications, and improved throughput will stand out.
Finally, commercialization strategies are becoming regionally tailored. Drivers of adoption in North America differ from those in Europe or Asia, where reimbursement models and regulatory pathways vary. The most successful companies will be those that adapt commercialization to the local context rather than applying a one-size-fits-all playbook.
Looking ahead
The story of 2026 will ultimately be about convergence. Technology advancements like imaging will overlap with changing commercialization models and new hospital realities to enable entirely new patient impacts and economic models.
Together, these shifts point to a future where surgical robotics is not defined solely by large machines in the OR, but by more intelligent, more flexible systems that integrate seamlessly into clinical workflows, deliver measurable value across diverse care settings, and keep pace with the rapid cycles of innovation that define modern healthcare.
For innovators, clinicians, and patients alike, that is a future worth anticipating.
Photo: PhonlamaiPhoto, Getty Images
Jian Zhang is a serial entrepreneur. Prior to Noah Medical, Jian also co-founded two other successful startups and served as the CEO. In addition, he was employee #2 at Auris Health, which was acquired by Johnson & Johnson for $5.7B in 2019. Prior to joining Auris, he worked at Intuitive Surgical. Jian received his MS and PhD from Columbia University.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.








