Something important happened in Florida on July 1st that most healthcare professionals probably missed — the state quietly passed a law allowing physicians to offer patients certain stem cell treatments that have not yet been approved by the FDA, for use in treating specific indications and subject to regulatory compliance.
Across the country, clinicians, patients, and policymakers are watching closely. Many see this as a long-overdue step toward expanding treatment options for patients that are not satisfied with the current standard of care.
As the demand for stem cell therapies continues to grow worldwide, Florida’s Senate Bill SB‑1768 is expected to bring about many differing options across the entire ecosystem. For physicians, it introduces an opportunity to offer patients new treatment alternatives while also putting a spotlight on the complex intersection of innovation, oversight, and clinical ethics, especially in a space that has long lacked regulatory clarity.
What the law actually allows
The law boils down to this: licensed physicians in Florida can now use non-FDA-approved stem cell therapies within the scope of practice for such physicians and for therapies that are related to orthopedics, wound care, and pain management. Compliance, however, is tightly regulated.
The sourcing requirements alone are quite stringent. Physicians must make sure that the biologics supplier they choose uses afterbirth placental perinatal stem cells, or human cells, tissues, or cellular or tissue-based products, all obtained in an ethical manner, and that do not involve stem cells derived from aborted fetuses. In addition, the stem cells must be retrieved, manufactured, and stored in a facility that is registered and regulated by the FDA, and accredited by the AABB, NMDP, or AATB. They must follow current Good Manufacturing Practices (cGMP) and retain post-thaw viability reports for each treatment lot. Plus, any marketing materials must clearly state that the therapy isn’t FDA approved. It cannot be buried in fine print. Choosing the right supplier is essential for physicians to stay compliant.
Patient consent represents another significant requirement. The law mandates detailed informed consent documents that spell out risks, alternatives, and regulatory status.
The risks of noncompliance
The consequences for cutting corners are steep. According to the bill’s official analysis, violations such as misrepresenting treatments, using fetal or embryo-derived cells, or failing to choose a biologics supplier who meets sourcing standards could result in felony charges and license revocation. While the law is state-specific, its implications are national as other states are expected to follow Florida’s initiative.
For physicians, this creates both opportunity and obligation. There is now more room to innovate, but also more pressure to ensure treatments meet high standards for safety, science, and transparency. In this environment, partnering with the right supplier is essential for safety. That includes verifying the scientific integrity of any product used and maintaining clear documentation and consent protocols.
As noted by New Regen Ortho, some products marketed as stem cell therapies contain little or no viable cells. Even with post-thaw viability documentation in place, therapeutic value depends on how the cells are sourced, handled, and delivered. The burden of quality assurance will continue to fall on providers, which is why choosing the right supplier is essential to meet this regulatory standard.
What this means for the market
Stem cell therapy has long existed in a gray zone, caught between scientific promise and regulatory gaps. Some providers operate with strong data and clear protocols, while others rely on marketing that outpaces clinical evidence.
SB‑1768 introduces structure where there was once ambiguity. By requiring more transparency around sourcing, consent, and advertising, the law will elevate providers who are already committed to responsible care. In addition, opportunities to expand the use of stem cell therapies and obtain data surrounding these treatments may provide a faster and cheaper pathway to develop and improve these therapies.
What physicians everywhere should take away
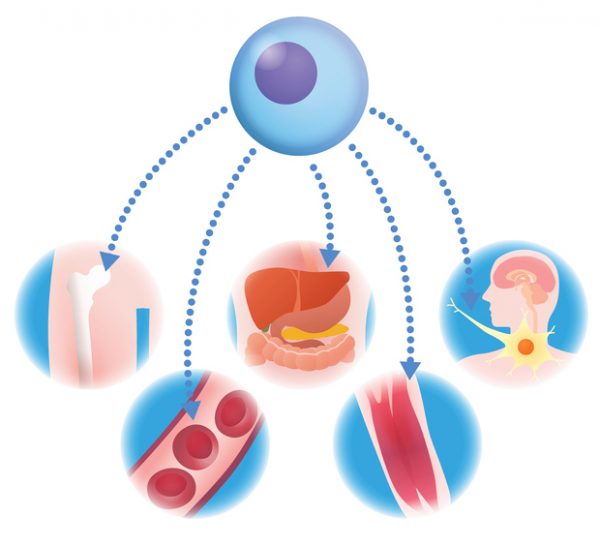
You don’t have to practice in Florida for this law to matter. Patient interest in regenerative care is growing rapidly, and physicians across the country need to be prepared to understand and consider advising patients, where applicable, of these stem cell-related treatment options. As the use of stem cells becomes more commonplace, the patient demand will increase, the science will continue to improve, and the cost of treatment will go down (it may even be covered under national health insurance plans in the future).
Innovation requires accountability
As other states consider following Florida’s lead, the responsibility falls on providers to push the movement forward. Access means little without accountability. Whether in Florida or elsewhere, patients deserve therapies that are as transparent and trustworthy. For physicians, the challenge is not just navigating what’s allowed, but making sure the source of the therapeutics is from reliable, diligent, and compliant suppliers.
Photo: chombosan, Getty Images
Ian Bothwell is currently the Chief Executive Officer and Chief Financial Officer and a member of the Board of Directors of ZEO ScientifiX, Inc., a publicly traded clinical-stage biopharmaceutical company (OTCQB “ZEOX”) focused on the research and development of biological therapeutic platforms and is currently positioning itself to be a leading provider of stem cell products for physicians in Florida that comply with the regulations of the new Florida legislation SB 1768.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.











