
From improving outcomes for vulnerable, post-acute patients to building collaborative networks using real-time data for measurable impact, it can take several different approaches to deliver quality care and get reimbursed in the world of value-based care. In an interview, Steve Holt, VP Government Affairs, PointClickCare, discussed how hospitals and ACOs can succeed with alternative payment model (APM) programs such as AHEAD, TEAM, and ACO REACH to reshape quality benchmarks.
CMS wants every individual with Medicare to be a part of a managed care program by 2030. This goal has spurred the development of Alternative Payment Models, under the CMS/CMMI banner, to figure out how to bend the cost curve without sacrificing quality along the way -– one of the biggest dilemmas in care delivery.
Holt said the TEAM model has paved the way for newer APM models.
“The TEAM model, specifically, is really the first instance of a large-scale government-mandated alternative payment model across provider types. It is a very strong indicator of the trajectory that we’re on with these models. It is safe to assume that these alternative payment models are very much going to continue to be the direction we go as fee-for-service continues to be less and less of the reimbursement pie.”
Holt says penalties for underperformers will likely take the form of sticks. It is critical to understand the importance of being an active participant, building the right relationships and focusing on delivering the best care possible.
“When you take a closer look at the TEAM model, which is focused on high-risk, episodic care packages, I’ll say it becomes even more important to figure out how to make sure that these high-cost bundles of treatments are managed effectively and efficiently. Most importantly, once the care begins beyond the four walls of a hospital or surgery center, how is care being delivered?”
Virtual care and effective care coordination solutions have an important role to play. The risk is if you’re not at the forefront, and you’re not actively involved in thinking about implementation and building relationships in your network as part of your health system strategy, your organization will be left behind. If that happens, it’s going to be extremely difficult to catch up once these alternative payment models become commonplace.
So where should hospitals and ACOs focus to improve outcomes for vulnerable, post-acute patients? Holt identified care transitions as one area where the healthcare industry has had difficulty because transition of care from a hospital or other acute setting to a skilled nursing facility, rehabilitation center or home environment can create a “black hole” of data. In these circumstances, it can be tough to work with partners to monitor a patient’s health, whether they are getting better, and whether care is being delivered appropriately and efficiently. Deploying technology and processes to improve communication beyond the walls of a hospital or other facility to augment and enhance care coordination is critical in these situations.
Hospitals need to build tighter partnerships with their downstream post-acute care providers, to ensure seamless information sharing and coordination. This starts with detailed discharge summaries and accurate medication reconciliation. It also includes being able to show when and where the patient is being referred to in order to reduce the clinical administrative burden for those care teams upon admission. In this way, healthcare providers can deliver care in a proactive manner, rather than reacting to a patient’s changes in health, according to Holt.
In a post-acute setting, such as a skilled nursing facility, assisted living facility or home health setting, engaging the patient and their families is critically important. They need to be aware of the loved one’s treatment plan and discharge instructions. They’re having conversations around social determinants of health and social needs to avoid unnecessary readmissions. It’s really about identifying how these care teams work together effectively rather than trying to completely redesign workflows between care settings that might not integrate together seamlessly.
“Innovation is paramount to an effective care delivery model where so often, transitions of care are the leading indicators of negative outcomes and the most significant cost drivers,” Holt noted, adding that as alternative payment models like TEAM and AHEAD expand, he believes bringing together communication, a well-trained workforce, and technology will be the biggest differentiator in this era of shared risk and connected care.
“I’ve really wanted to focus on the importance of communication, workforce and technology. Those three things have to be working effectively and efficiently together to succeed, whether or not you’re in an alternative payment model,” Holt said
CMS has established tougher benchmarks to help hospitals and ACOs improve quality of care and costs. Holt outlined some practical strategies hospitals and ACOs should use to meet these new expectations—especially when caring for high-risk, post-acute patients.
Three key things are needed, according to Holt. First and foremost, effective communication between the different care delivery settings is a must.
Second, the hiring and training of workforces within those different care settings must be enhanced so they can thrive and perform the best care possible. Third, their work must be augmented through technology investment, making sure that the best tools possible are at their fingertips. The patients in these care settings tend to be high risk and high cost.
Holt also advocated for increased technology investment in the senior and behavioral health care settings to enable better cross-continuum collaboration.
“We utilize discharge summaries from our skilled nursing facilities that automatically get sent to the Emergency Department (ED),” Holt said. “If that patient is discharged and shows up in the ED again, those ED care teams already have complete visibility into where that patient is coming from, why that patient is presenting in the ED, and they’re able to really jumpstart that care delivery once the patient is admitted.”
Alternatively, when a patient is discharged from an emergency department and sent to a skilled nursing facility, PointClickCare’s tools help populate that patient record and ensure that pertinent information is available for the skilled nursing facility care teams. It makes the patient onboarding process seamless, Holt said.
Holt noted that PointClickCare can be used to set up an alternative payment model or risk-based model for a cohort of patients to track against CMS APM benchmarks to generate the results these APMs need. Its tech can also be applied to assisted living in support of a patient’s treatment plan.
Holt offered an example focused on medication management for patients.
“If you look at the average senior who is admitted to a skilled nursing facility, they are on 11-12 prescribed pharmaceuticals. One part of the solutions that we bring to the table is making sure that as the patient’s data comes through the EHR, it auto populates into the patient record that the clinician sees. One common error that happens when clinicians manually enter data is incorrect drug information may be accidentally entered. This is the kind of error that not only can lead to a complication requiring an emergency department visit, it can deliver a setback to an elderly patient’s health from which they may not easily recover.”
Holt pointed out that interoperable communication is vital to ensure crucial patient data can be exchanged between care teams seamlessly and in a time-sensitive manner.
In these care transitions, where care teams need to proactively manage high-risk patients to avoid needless readmission, predictive analytics tools have a critical role to play, Holt emphasized.
“EHR systems can make it easy for care managers, whether they are with an ACO, the health system or a risk-bearing entity. We need to make our tools as user friendly as possible, so that the caregivers are not spending endless amounts of time dealing with tech as opposed to delivering the actual care,” said Holt.
Congress enacted the HITECH Act in 2009 to promote investment in tech supporting interoperability between healthcare organizations. The move also established Meaningful Use requirements, requiring healthcare organizations to share patient data between ambulatory and acute care settings.
But the HITECH Act overlooked investment in the entire senior care continuum and the behavioral health care continuum, Holt observed. As a result, said Holt, “you’ve seen a significant divergence of technological sophistication between care settings, and this is what’s led to dramatic fragmentation of IT systems. It is why you don’t necessarily get seamless communication between the care settings. Rectifying that is one of PointClickCare’s priority advocacy efforts.”
To realize the goals of value-based care, innovation and collaboration are critical to helping alternative payment models succeed. Having a reliable technology partner is essential for success.
This box breaks down the Alternative Payment Models discussed in this article:
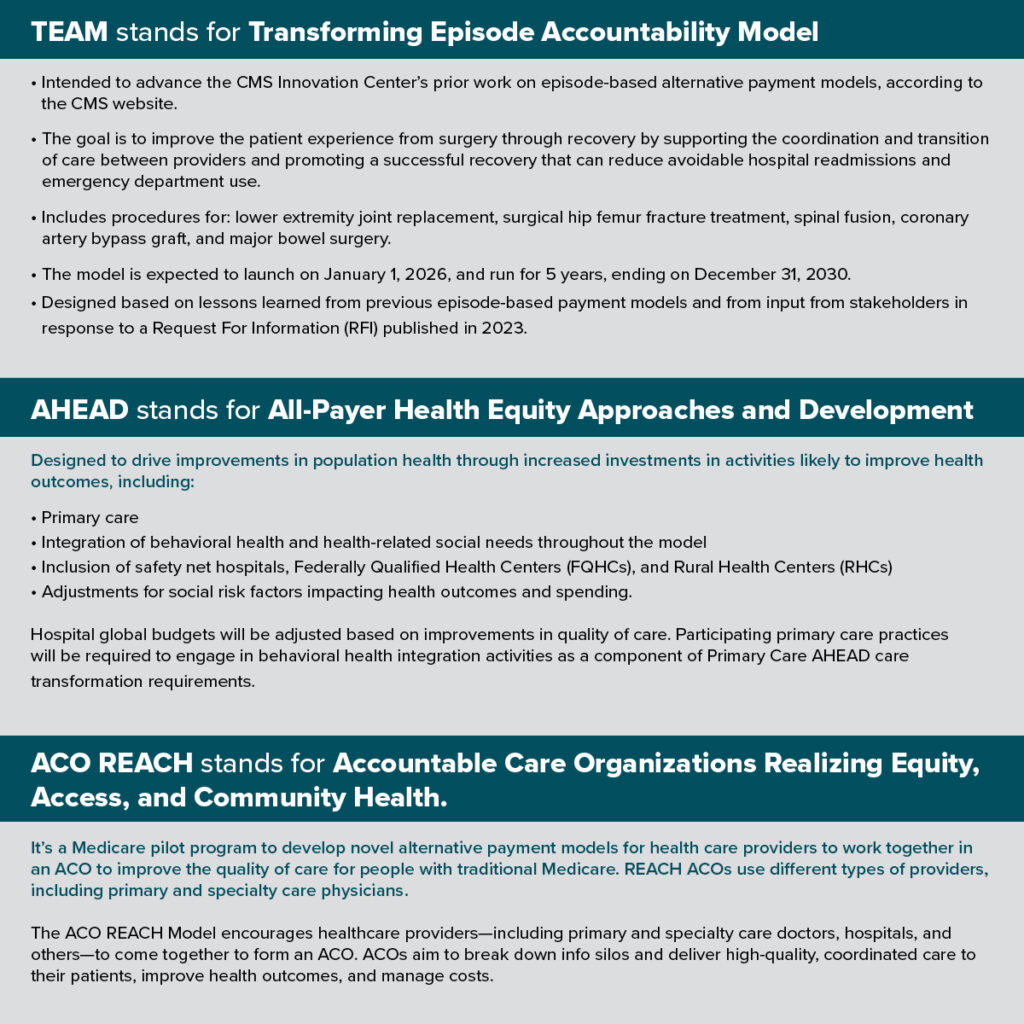
Photo: Supatman, Getty Images







