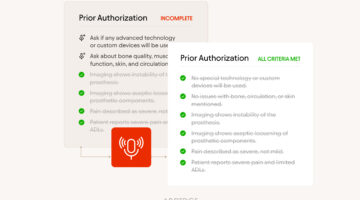
Choosing the Right Methods for the Right AI to Accelerate Prior Authorizations
With regulatory scrutiny intensifying and the demand for speed, compliance, and clarity growing, understanding the nuanced differences between AI approaches is essential for payers, providers, and patients alike.