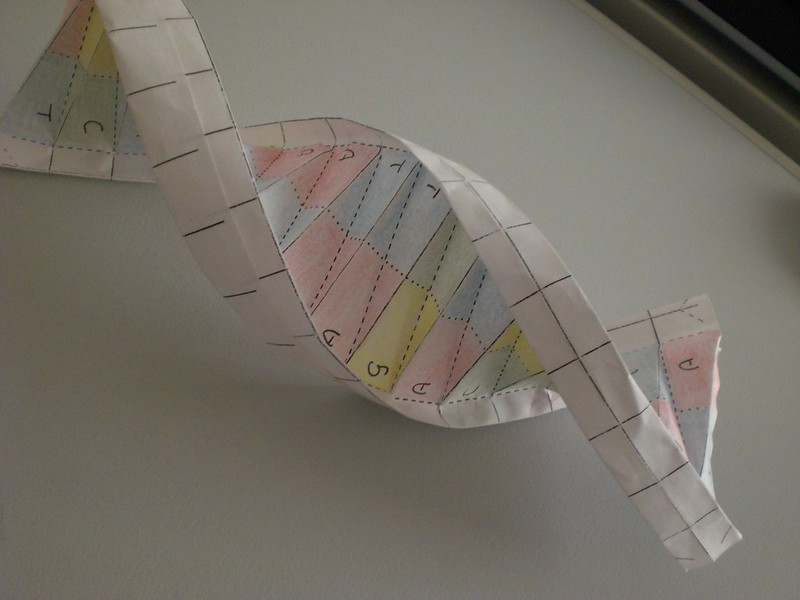
In the medical research realm, few things currently generate as much excitement as regenerative medicine’s potential. Right now, scientists are conducting translational research and studying lower-level species that can already regenerate damaged tissue and organs to understand how it happens.
On top of that, researchers are looking into genetic pathways that cultivate physiological and pathological human cell regeneration. Those studies are aided by four ongoing nonhuman research efforts that demonstrate the promise of human regeneration and open the door to progress on multiple fronts.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
Zebrafish Cell Regeneration
With the ability to regrow entire fins, zebrafish are among the most regenerative creatures on the planet. In fact, Duke University researchers successfully injected zebrafish embryos with proteins that color each scale a unique hue.
This assists scientists in tracking each scale’s development and studying how fish recover and regenerate scales when tissue is damaged. Research found that zebrafish cell growth accelerates 50-100 percent to replace lost tissue.
It’s believed that because lower-level organisms like zebrafish have vast regenerative capabilities, higher-order organisms should have similar, albeit inhibited, capabilities. If we can understand how zebrafish regenerate cells, we can perhaps translate this capability to humans.
Newt Retinas
Human retina cells are efficient self-healers. Retinal pigment epithelium (RPE) cells respond to trauma by multiplying and migrating to heal wounds. However, this reaction produces a side effect: proliferative vitreoretinopathy, a retinal disorder that causes a loss of vision.
Adult newts don’t have this problem. When a newt’s retina is damaged, it and the RPE are completely restored, healing the damage and restoring vision.
A study by the University of Tsukuba in Japan showed that inhibiting the Pax6 protein in newt stem cells caused RPE cells to function like they do in human retina, healing wounds but not vision. Human retinas also possess this protein, something scientists hope will lead to discovering how to control the mechanism that enables Pax6 to heal and restore vision in humans.
We are just at the beginning of our understanding of the role proteins play as messengers in the human body. While some uncertainty exists around the activation of specific pathways, newt retina findings add to our understanding of organ regeneration.
Human Kidney Regeneration
Human embryos generate anywhere from 500,000 to 1 million nephrons — minute kidney waste filters— in the first three months of gestation. After this point, more nephrons can’t be created, and any serious loss of nephron functionality yields kidney failure.
Researchers at The Saban Research Institute of Children’s Hospital Los Angeles isolated the human nephron progenitor (NP) cells that produce nephrons to shed some light on possible causes. Coming out of the study, using NP cells to regenerate nephrons and restore kidney function in humans with kidney failure was deemed a possibility.
We know every cell contains the blueprint for the entire human body. The challenge is to unlock the potential of this information to spur the regeneration of specific cells. In particular, this is a major step in addressing the ongoing challenges kidney failure presents.
Worms and Immune System Management
Immune systems work in mysterious ways. In humans, our immune systems release bacteria in the microbiome that, depending on the situation, can accelerate or block healing. This is especially problematic in wound recovery; normally, when the body decides a wound is beyond repair, it produces bacteria to impede recovery.
Scientists at the Stowers Institute for Medical Research and the Howard Hughes Medical Institute found that flatworms — which can regenerate anything, including their entire heads — lose their regenerative powers when infected. The same study found that when a specific gene called TAK1 kinase was blocked, the infected flatworms were able to recover and regenerate in spite of the infection.
Researchers believe that the worms’ immune systems used the TAK1 pathway to rid themselves of infected cells so the virus couldn’t spread. It may be possible to find the genetic pathways in the human immune system that block cell destruction and foster self-regeneration.
Immune responses are closely connected to the healing mechanisms of the human body, including scar formation and wound closing. Understanding and possibly controlling immune response is important for human regeneration, especially considering that the protective mechanisms of the immune system can sometimes inhibit regeneration.
Broad Implications
In the not-too-distant future, we may see the standards of care for many illnesses transformed from reactionary loss prevention — stopping the loss of the body’s function — to the regeneration of full functionality and health.
Regenerative medical research is taking place on many fronts because there are multiple pathways to stimulate human organ and tissue growth. The research will continue to advance, with or without success, and will eventually mature into a series of standardization efforts.
Imagine if people could heal faster and more completely by using their own bodies instead of invasive procedures such as transplants or organ removal. This has the potential to dramatically improve outcomes, extend lives, and lower healthcare costs worldwide.
Photo: Sigrid Gombert, GettyImages