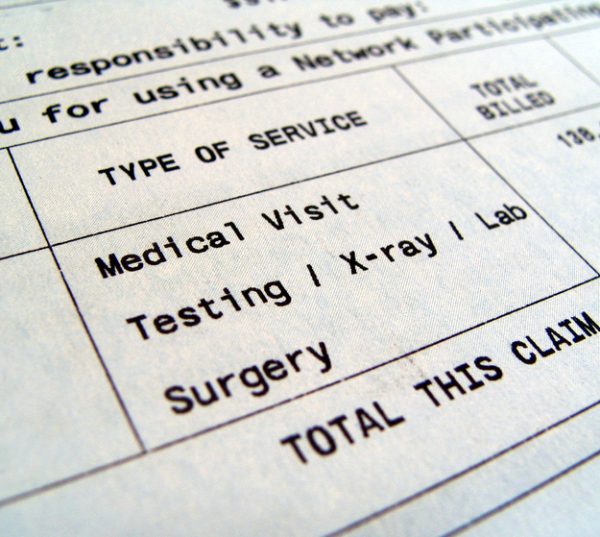
Legislators advanced a new proposal that would protect patients from surprise medical bills. The Ban Surprise Billing Act passed the House Education and Labor Committee on Tuesday.
Patients are subject to “surprise bills”, or balance billing, when they receive care from an out of network physician. They’re billed for the difference between what their insurance paid and the total cost of care.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
While surprise bills are often thought of in the context of emergency surgery — such as having an out-of-network anesthesiologist — a study published Tuesday in JAMA showed more than 20 percent of patients faced unpaid bills after an elective surgery.
Similar to previous, bipartisan legislation at the end of 2019, the Ban Surprise Billing Act would allow providers to bill patients an amount equivalent to median in-network rates to resolve out-of-network payments. Bills above $750 would go to arbitration. Committee Chairman Bobby Scott (D-Va.) and Rep. Virginia Foxx (R-N.C.) are co-sponsors of the bill.
But the legislation will face similar challenges to last year’s efforts, when legislation stalled after a lobbying storm by physician groups and emergency services companies.
Hospitals and provider groups have said the bill could have consequences beyond surprise bills, affecting providers’ negotiations with insurers.
In a letter to Scott and Foxx, the American Hospital Association wrote that the legislation would remove incentives for health plans to contract with providers and could depress in-network rates.
“We strongly oppose approaches that would impose arbitrary rates on providers, which could have significant consequences far beyond the scope of surprise medical bills,” AHA CEO Richard Pollack wrote.
Hospitals and providers support a separate, rival bill proposed by the House Ways and Means Committee that would send all payment decisions to an arbitrator, who would consider payers’ median in-network payment rates.
“We support the underlying mechanism for resolving these disputes, including the eligibility of all disputed claims for negotiation and mediation,” AMA President Dr. Patrice Harris wrote in a statement. “We also appreciate that the mediator must consider a wide range of supporting information submitted by physicians in rendering a final determination.”
Even with that bill, the AHA requested that mediators only consider rates set between commercial health plans and providers, rather than lower federal reimbursement rates.
The Congressional Budget Office has estimated the bill would reduce the federal deficit by $5.47 billion in the next five years, assuming average payment rates move closer toward the median in-network rate.
Photo credit: Ibodvar, Getty Images














