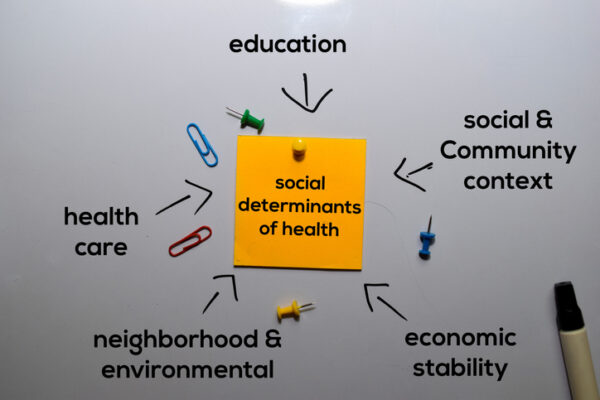
It is widely recognized that socioeconomic factors have a profound impact on health outcomes. Addressing these social determinants of health (SDOH) is an essential part of “total care,” with physical and behavioral healthcare being the other primary components. However, this calls for a deep understanding of how these elements are interconnected, and from a practical standpoint, requires concerted focus and capacity to remove social and economic barriers standing in the way of better health outcomes.
None of this is easy even in the best of times. It has become far more challenging during the Covid-19 public health crisis, even as the pandemic brings into sharp focus the importance of addressing SDOH. People with underlying health conditions have experienced the worst outcomes of Covid-19, and we know that lower incomes are tied to higher rates in chronic illnesses. Populations that were already struggling at the intersection of poor health and economic insecurity now face a greater need for food, transportation, and medical and behavioral healthcare, even while these resources have become increasingly strained.

Behavioral Health, Interoperability and eConsent: Meeting the Demands of CMS Final Rule Compliance
In a webinar on April 16 at 1pm ET, Aneesh Chopra will moderate a discussion with executives from DocuSign, Velatura, and behavioral health providers on eConsent, health information exchange and compliance with the CMS Final Rule on interoperability.
Much of the healthcare system, especially in urban areas, is currently working in overdrive mode to meet the demand created by Covid-19. As the pandemic spreads to more rural areas, the situation could become even more dire. Healthcare resources have long been severely constrained in rural America. Within the past decade, 120 hospitals have closed in rural areas, and 1 out of every 4 remaining are in danger of following suit.
Shelter-in-place orders have led to widespread financial hardships and unemployment, leaving millions of Americans without an income. For those who were already meeting poverty level thresholds, it means the precious few outside resources available are being spread across a much wider population.
To an important degree, technology can help address these social determinants of health (SDOH). It can identify who the high-risk vulnerable populations are, stratify within populations to determine those with the greatest need and discover resources to address that need. All of which is extremely valuable.
Yet technology alone, no matter how sophisticated, cannot solve all the issues facing Americans right now. For that, we still need humans and their capacity for compassion, resourcefulness and commitment.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
What humans bring
Here is an example of how those human qualities come into play. Recently, a care coach coordinator in Texas attempted to use the “211” system to help a family gain needed access to food. Despite multiple phone calls, she was never able to reach a live person.
A machine likely would have persisted going down the same avenue, contacting the same resources with the same results, or might have been programmed to stop after three attempts. The care coach, however, understood the urgency of the need, and instead persisted for four relentless days. She went outside the typical boundaries of her program until she finally located a church 30 miles away who generously dispatched a volunteer to deliver food to the distressed family.
The lesson here is that addressing social determinants of health at any time, but especially during a pandemic, requires compassion and persistence to make the exhaustive outreach until a family is connected to lifesaving resources.
The impact of SDOH
Maslow’s Hierarchy of Needs explains very clearly why SDOH issues are such an impediment to healthcare. The most basic human needs are for air, food, drinkable water and shelter. Our brains are wired to prioritize these issues above all others, which means if they are not first addressed, we have little ability to focus on higher-level issues such as healthcare or what to do to limit our exposure during a pandemic. In other words, if the choice is between obtaining food for ourselves and our families or ensuring we avoid exposure to a virus that may or may not affect us, food will win every time.
This same thinking is also at play during non-pandemic times, incidentally, which explains why it is so difficult to get populations with SDOH and/or behavioral health issues to participate actively in their own healthcare.
Those who are most vulnerable to economic stress during a pandemic also tend to have multiple chronic conditions, often as a result of their environments. For example, a high density of fast food and convenience stores with a corresponding low density of quality food options in poor counties can quickly lead to diabetes, obesity, heart disease and other chronic conditions, individually or in tandem.
Not just an urban issue
While SDOH issues are often thought of in an urban context, many rural communities have older populations with higher rates of chronic lower respiratory disease and hypertension.
Non-metro communities also tend to have higher poverty rates than metro areas (16.1% to 12.6%). This is an issue because of the connection between socioeconomic factors and health. At the same time, the rural culture of self-sufficiency, ingrained over centuries, tends to make people in these areas less-inclined to reach out for help, creating additional challenges when dealing with SDOH issues.
In a pandemic, the factors that lead to a lower level of health are amplified. Overcoming these barriers to care requires more than simply identifying who has need. It requires empathy, compassion and finesse to help people understand that receiving assistance in their time of need is not an admission of failure or weakness but rather a path to avoid a poor outcome.
Keeping the system from becoming more stressed
Helping members avoid Covid-19 is not the only benefit of managing SDOH more effectively, although it is an important one. Keeping non-Covid-19 cases out of the emergency department (ED) or inpatient stays frees beds, clinician time, personal protective equipment (PPE) and other resources to deal with the pandemic. It also lowers the risk of these very vulnerable members from being exposed to the virus when they would not have been otherwise.
Of course, it also reduces the cost to health plans. The annual medical cost for people with chronic conditions averages around $33,000 when they also have untreated behavioral health issues. Those costs decrease by 50% or more when the behavioral issues—often driven by SDOH challenges—are addressed.
Getting members to admit they have these issues, however, can be difficult. That is why skilled engagement specialists are so important. They can build the trusted relationships needed to understand what it will take to turn those solutions into action.
Take the earlier example. Had the church not been able to deliver the food, and had the family not been able to send someone to pick it up, there is a strong possibility a technology-only approach would have seen that as an impasse. The addition of a compassionate, persistent care coach paved the way for the food to be transported from the church to the family. This resolved the issue and enabled the family to focus on staying healthy rather than avoiding hunger.
The human touch
While it seems paradoxical to talk about the human touch in a time of social distancing, it is clear that successfully managing SDOH issues during a pandemic requires, in addition to technology, creative thinking and a passion for resolving whatever challenges arise.
When paired with genuine empathy for the needs of another person, this combination of technology and human intervention can be a powerful weapon in the battle to overcome not just the current pandemic but all the barriers to better health.
Photo: syahrir maulana, Getty Images
Julia Wright, MD, is Chief Medical Officer at Catasys. (NASDAQ: CATS), a leading AI-powered and telehealth-enabled, virtualized outpatient healthcare treatment company.












