
The stress of long lockdowns, job losses and other worries due to the Covid-19 pandemic is taking its toll on Americans. According to the results of a recent Kaiser Family Foundation poll, 53% of adults said their mental health had been negatively impacted due to worry and stress over Covid-19, up from 32% in March.
Respondents also reported other health effects, with more than a third of adults saying they had difficulty sleeping. Others reported difficulty eating, worsening chronic conditions, and increases in alcohol consumption or substance abuse.
These challenges are on top of existing shortages of mental health providers. A report by United Way of the National Capital Area pointed out states with a high ratio of residents for every mental health provider. For example, in Alabama, there were 990 residents per one mental health provider. In Texas, there were 880 residents per provider.
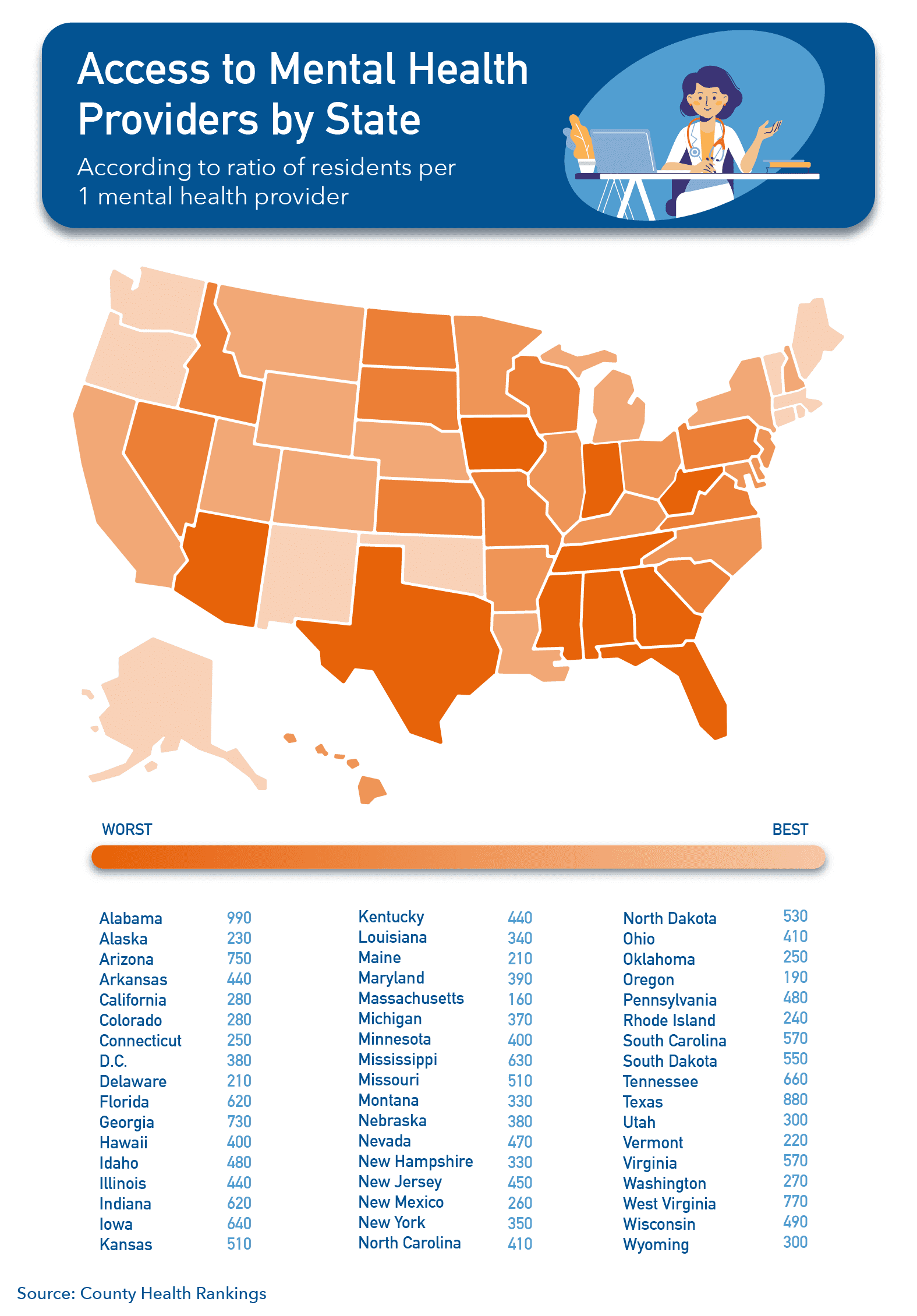
A report by United Way of the National Capital Area shows which states have the highest ratio of residents to mental health providers. Data from the Robert Wood Johnson Foundation’s County Health Rankings.
United Way also surveyed 2,500 people about how they felt about accessing mental healthcare, and if telehealth changed that.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
Overall, 34% of Americans said they felt comfortable accessing mental health resources, while 22% said they felt uncomfortable (23% indicated neither).
When it came to telehealth appointments, surprisingly, only 26.7% of respondents said they felt more comfortable accessing mental health services. Another 27.7% of respondents said they more uncomfortable accessing virtual care, while many — 45.6% — said it didn’t affect their comfort level at all.
Photo credit: Aleksei Morozov, Getty Images













