A year of uncertainty, high levels of stress and unrelenting demand for care has left the mental health of healthcare workers in tatters.
Despite three-fourths of healthcare workers saying that they feel “hopeful” when going to work these days, about half also say they feel “burned out” (55%) or “anxious” (49%), according to a poll conducted between Feb. 11 and March 7.
Administered by the Kaiser Family Foundation and The Washington Post, the survey includes responses from 1,327 frontline healthcare workers.
A majority of healthcare workers (62%) say that the worry or stress related to Covid-19 has had a negative impact on their mental health, according to the survey. More than half (56%) of all respondents say that the stress has caused them to experience trouble with sleeping or sleeping too much (47%), frequent headaches or stomachaches (31%), or increased alcohol or drug use (16%).
Younger healthcare workers appear to be feeling pandemic-related stress and anxiety more than the older age groups. About 40% of healthcare workers, 65 years and older, report that the pandemic has had a negative impact on their mental health, as compared with 75% of those aged 18 to 29.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
Though only one in six healthcare workers say they tested positive for Covid-19, about 80% say that concern about being exposed to the coronavirus at work and exposing others in their household have been sources of stress during the past year, the survey shows.
Approximately 13% of healthcare workers say they have received mental health services or medication due to the stress related to Covid-19, and an additional 20% say they thought they might need such services but did not get them.
The reasons for not getting mental healthcare varied, with 27% saying they were too busy to seek it, 16% saying they couldn’t afford it and 14% saying they couldn’t get time off work, according to the survey.
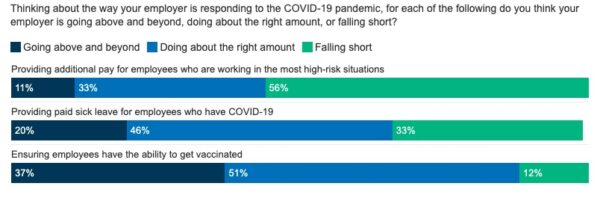
Though healthcare organizations are providing benefits to help their employees through this challenging time, they are not doing enough on at least one front, healthcare workers say.
Most respondents said their employer is “doing about the right amount” or “going above and beyond” in terms of providing sick leave to employees who had Covid-19 (66%) or ensuring employees have the ability to get vaccinated (88%). But 56% said they are “falling short” when it comes to providing hazard pay, which is additional pay for performing a hazardous duty or work involving physical hardship.
Now that the vaccine rollout is well underway, a majority of healthcare workers (81%) say that the pandemic is completely, mostly or somewhat under control.
But this view varies across racial groups. About 31% of Black healthcare workers say that the outbreak is not at all under control, as compared with 15% of white workers.
Photo: Ivan-balvan, Getty Images, Kaiser Family Foundation/The Washington Post survey