The Department of Health and Human Services, along with two other agencies, have issued the first set of regulations implementing the No Surprises Act, which was enacted into law at the end of 2020.
The interim final rule released on Thursday will restrict surprise billing — which is when patients are charged for out-of-network care, often unexpectedly — for Americans insured through employer-sponsored and commercial health plans. Issued by HHS, the Departments of Labor and Treasury, and the Office of Personnel Management, it will take effect Jan. 1, 2022.
The rule bans:
- Surprise billing for emergency services.
- High out-of-network cost-sharing for emergency and non-emergency services.
- Out-of-network charges for ancillary care at an in-network facility in all circumstances.
- Other out-of-network charges without advance notice.
“No patient should forgo care for fear of surprise billing,” said HHS Secretary Xavier Becerra, in a news release. “Health insurance should offer patients peace of mind that they won’t be saddled with unexpected costs.”
Per the new rule, out-of-network rates for providers, including any cost-sharing, will be determined by an applicable All-Payer Model Agreement or state law. If there is no applicable agreement or specific state law, the provider will receive an amount agreed upon by the payer and provider or by a third-party arbiter.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
The No Surprises Act provides for a negotiation period during which providers and payers can settle out-of-network claims. But, if they cannot reach an agreement, they enter into a binding arbitration process, where an independent arbiter will help make the final payment decision.
The newly issued rule does not include any regulations concerning arbiter entities or the arbitration process. Those will be released “soon,” according to a fact sheet released by the Centers for Medicare & Medicaid Services.
The rule has not been finalized, and the agencies that issued it are inviting comments for 60 days after it is published on the federal register.
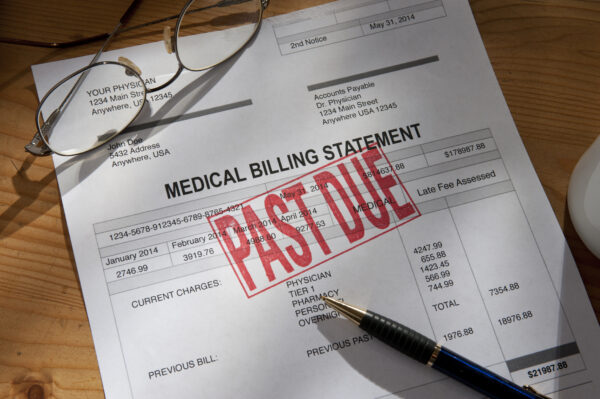
Unexpected healthcare bills are a major source of concern for the American public. About two-thirds said they worry about being able to afford surprise medical bills, a 2020 Kaiser Family Foundation report shows. And the concern is not unfounded — 66.5% of all bankruptcies are linked to healthcare expenses.
Curbing surprise medical bills is also one of the few truly bipartisan issues in healthcare, with a majority of both Democrats and Republicans supporting government action to protect patients from these expenses.
The industry has been less supportive. An earlier version of the No Surprises Act released last December drew criticism from both provider and payer organizations.
Photo: KLH49, Getty Images












