In the landscape of mostly injectable Covid-19 vaccines and therapeutics, Meissa Vaccines stands out with its intranasal approach. The company contends that the more patient-friendly dosing option isn’t its only advantage. Easier and more economical to manufacture and store, global distribution of an intranasal vaccine should be less complicated, according to CEO Martin Moore. Crucially, the way Meissa’s vaccine works could also make it better than injectables at blocking viral transmission.

Behavioral Health, Interoperability and eConsent: Meeting the Demands of CMS Final Rule Compliance
In a webinar on April 16 at 1pm ET, Aneesh Chopra will moderate a discussion with executives from DocuSign, Velatura, and behavioral health providers on eConsent, health information exchange and compliance with the CMS Final Rule on interoperability.
“We have some tools, but we don’t have transmission-blocking tools,” Moore said of the field of authorized Covid-19 products. “Until we do, we’re going to be playing catch up.”
A Phase 1 study testing Meissa’s vaccine is already underway and is expected to report data later this year. But Meissa now has data from monkey studies that the Redwood City, California-based company says are an indicator of how its vaccine could work in humans. Results released Monday showed that a single dose provided protection against the novel coronavirus comparable to the efficacy reported in monkey studies evaluating currently authorized vaccines.
The vaccine candidate, MV-014-212, elicited antibodies against the novel coronavirus as well as two variants of concern. In addition to antibodies that circulated systemically, the data also show that the vaccine induced mucosal antibodies in the upper respiratory tract. That’s important because the respiratory system is the major infection route of the virus, and stopping the virus there is key to stopping transmission, Moore said. The data are scheduled to be presented on Thursday during the American Society of Virology’s annual meeting, which will be held virtually.
Injectable vaccines induce antibodies in the blood, which protects against severe disease and hospitalization. In order to prevent against transmission, higher levels of antibodies are needed in the circulation to reach the mucosal surfaces of the nose—10 times higher than what’s required to protect the lungs, Moore said. Meissa aims to achieve those higher antibody levels by producing them right in the nose.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
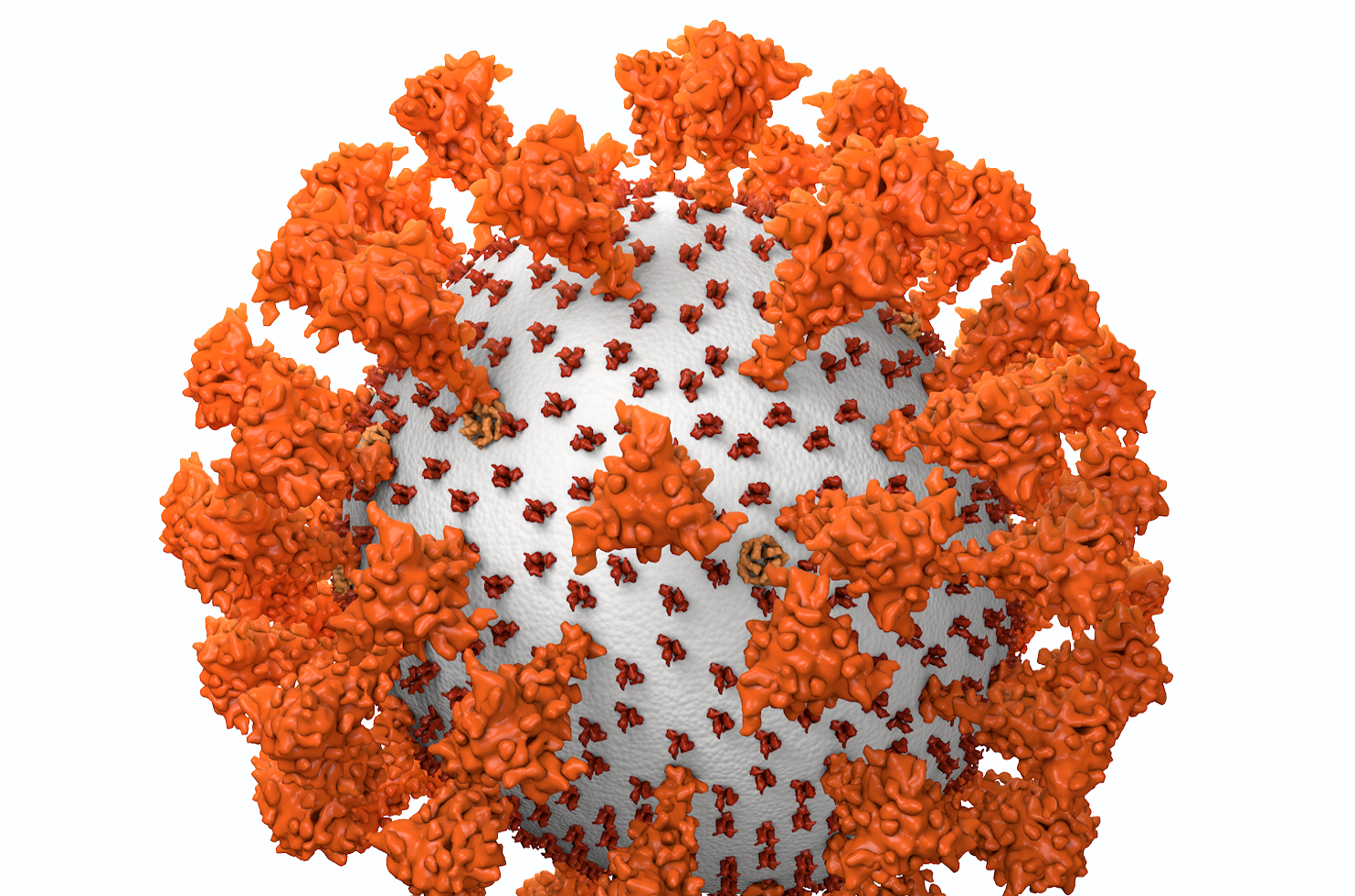
The Meissa vaccine candidate is a recombinant attenuated SARS-CoV-2 virus, which means it’s engineered to be more stable and better at producing an immune response. Live attenuated, or weakened, viruses are a more traditional approach to vaccination, leading to vaccines that are durable and provide broad immunity, Moore said. Unlike in mRNA vaccines, which produce spike protein in one shape, Meissa’s vaccine uses a spike protein that is fully functional on the surface. That surface reveals more epitopes, the parts of the antigen that are recognized by the immune system. Meissa does not know exactly the mechanism of its vaccine’s potentially broad immunity, but Moore said it could be because of the vaccine’s fully functional spike protein.
The challenge of any live, attenuated vaccine is striking a balance between weakening the virus so that it’s safe but not weakening it so much that it’s no longer able to produce an effective immune response. Meissa accomplishes both goals with synthetic biology techniques. The virus is genetically engineered to remove the virulence genes, resulting in a strain that does not cause disease, Moore said. This approach can attenuate the virus and improve its ability to confer immunity.
“That really opens up the window to make live attenuated strains that are more potent for their level of attenuation,” he said.
The Meissa technology, AttenuBlock, is based on about 10 years of Emory University research focused on developing an intranasal vaccine for respiratory syncytial virus. Meissa has already advanced an RSV vaccine candidate to clinical testing. When the pandemic struck, the company used its technology to produce a Covid vaccine candidate.
The Meissa Covid vaccine must be stored frozen, but not at the ultra-freezing temperatures required of the messenger RNA vaccines, Moore said. The company is researching a refrigerated version. Meissa is also testing a spray device for its vaccine candidate.
The potential advantages of intranasal products has drawn a handful of companies to pursue such vaccines, or apply existing intranasal research to Covid-19. Altimmune was already developing intranasal vaccines for anthrax and influenza when the pandemic hit. The Gaithersburg, Maryland-based company used its technology to produce an intranasal Covid vaccine candidate. But preliminary Phase 1 data released late last month showed the vaccine did not produce an adequate immune response, leading the biotech to stop work on that program.
The Altimmune respiratory Covid vaccine candidate was based on the company’s platform technology, which employs adenovirus that’s engineered so it does not replicate. Moore said that adenoviruses are not traditionally used for intranasal vaccines, and he does not see Altimmune’s clinical trial failure as having any effect on the prospects for Meissa’s intranasal vaccine.
Another startup pursuing an intranasal Covid product is Netherlands-based Leyden Labs, which emerged in March with €40 million funding. The company hasn’t disclosed many details about its research, other than to say it is developing a nasal spray intended to stop the virus in the respiratory tract. Leyden Labs’ goal isn’t to replace vaccines, but rather, complement them with a faster-acting product that stops the virus from infecting an individual and also prevents that person from transmitting the disease.
Meissa launched in 2019 backed by a $30 million Series A round of funding. That cash is supporting the startup’s Covid vaccine research. Moore said Meissa is preparing to take the Covid vaccine candidate forward on its own, but the company could also pursue partners that could accelerate its development. The Phase 1 study is enrolling about 130 people in the U.S. Phases 2 and 3 will be done in places in the world where there is more transmission and disease, Moore said.
In other recent Covid-19 vaccine news…
The FDA has formally accepted, under priority review, the Pfizer and BioNTech application seeking formal approval for their Covid vaccine candidate in those 16 and older. Priority review takes about six months, placing the target date for a decision in January of next year. But a decision could happen sooner, as the regulator said that review “has been ongoing, is among the highest priorities of the agency, and the agency intends to complete the review far in advance” of the goal date.
Image by Meissa Vaccines












