
The confluence of the social justice events and the Covid-19 pandemic have exposed fractures in our health system putting a spotlight on health inequities impacting our communities of color. This is no longer an issue that our fragile health system can set aside as a “to-do” later. Addressing health equity for Covid-19 testing, hospital care, access to vaccination and deferred treatment of pervasive chronic diseases must become a national priority, which can be handled through private and public partnerships.
In order to fully understand the impacts of Covid-19 on our communities of color, we must acknowledge the historic, structural, social and economic challenges that have persisted, which have inhibited the ability for communities of color to achieve prosperous healthy lives.
Recognizing that social determinants of health include social factors outside of the health system, we should strive to eliminate zip codes and poverty as key indicators of life expectancy. To achieve health equity, we must strive for an inclusive, fair distribution of resources and opportunities. That will translate to better experience for patients and improved health outcomes. To provide this, as an industry, we need to design culturally competent, digitally equitable health solutions that meet people where they are with empathy for individual needs at the core.
This means we must view health equity as a long-term investment that proactively moves upstream, past the individual and episodic care, to the community. Redefining returns on investment will be key to attracting the appropriate ecosystem partners who have a ROI mindset of six-to-ten years. One such-long term investment that has proven to be successful is Lift Orlando where they strengthened communities through transformative partnerships and investment.
We unquestionably have more work to do. For example, both the National Center for Biotechnology Information and AARP report that prescription labels translated from English to Spanish are often wrong or incomplete. Several studies have demonstrated that Black patients seen by Black doctors receive more preventative services. And the AAMC reportsthat 22% of Black patients are less likely to receive pain medication than others.
Such data underscores that we need to re-focus our healthcare delivery so that it puts an empathetic lens on patient’s true needs. Studies continuously demonstrate that preventative care can help stave off chronic illnesses, and that chronic illnesses are burdensome health costs. As an industry, we know we need to move our focus away from episodic health treatment to health plus wellness.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Rich Birhanzel Rich Birhanzel is a senior managing director responsible for Accenture's global healthcare business.
These are such big goals that it is fair to say many in the industry have viewed them as too big to tackle or it’s “not my responsibility”. But the pandemic has forced us to consider ways to address this – and we shouldn’t limit our thinking to just solving the present emergency.
As we roll-out vaccination services, leveraging nation-wide, regional or state-wide healthcare providers is proving essential. We are also seeing the role of major retail pharmacy chains that already have primary care capabilities shift to vaccinate more people; for many this could be a starting point to offer more continuous medical services and an improved experience to people. Those patients who perhaps never thought to seek care in a retail pharmacy may reconsider. Pop-up tents that have served as vaccination centers could also be a model for future care, ranging from run of the mill flu vaccines to bespoke services such as cancer screening – and these could therefore introduce new entrants into the competitive healthcare field.
Given we know the delivery of health is increasingly going to include digital services, and we know many communities still lack reliable, consistent internet access and smart phone services, digital access that augments – not replaces – physical access can improve equity. But even this will require working with local community leaders who can provide bridges towards a positive experience. For example, pairing up with a library or civic center for internet service and training local leaders to serve as liaisons is a starting point.
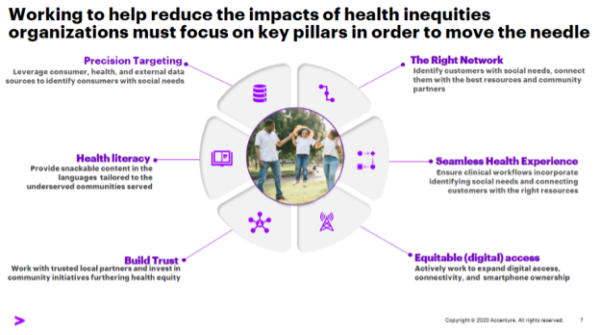
The leaders will be those that take bold steps to build the right networks, move past the safe pilots and leverage an “all hands-on deck” mentality to meet people where they are and to provide the greater access, experience and health outcomes they want. We must engage our community-based organizations and ecosystem partners in long-term relationships and seriously invest in them. Thinking innovatively and recognizing the digital divide as a guiding principle will be key to improving trusted, precision communication, engagement, that delivers equitable care and health literacy.
Delivering health equity is the right thing to do. Making healthcare more accessible and equitable is a moral obligation mandate that we as an industry should make sure remains on the cards.
Photo: PeterPencil, Getty Images
Rich Birhanzel is a senior managing director responsible for Accenture's global healthcare business.














