One of the hottest areas of cancer research involves a protein on cancer cells that keeps them cloaked from the immune system. Blocking this protein, CD47, is like ringing the dinner bell for macrophages, immune cells that munch on pathogens. The science of blocking CD47 as a way to get the immune system to target cancer cells led to Forty Seven, a biotech company that Gilead Sciences later acquired in a multi-billion dollar deal.
Amira Barkal, a physician/scientist, watched the development of Forty Seven while conducting Ph.D. research in the lab of Irving Weissman, the Stanford University stem cell biologist whose research led to the founding of that biotech and others. Barkal was not involved in Forty Seven, but she studied CD47 as it relates to other proteins that send out “don’t eat me” signals to macrophages. Barkal’s work in the Weissman lab led to the discovery of a promising new protein, CD24, with potential applications in breast and ovarian cancers. Now she’s the founder of her own biotech startup, Palo Alto, California-based Pheast Therapeutics.
“Irv has embodied this philosophy: For a bench discovery to make it to patients, the scientists involved have to be involved in the clinical development,” Barkal said. “That’s what we’re doing at Pheast.”
Pheast unveiled a $76 million Series A financing on Tuesday, a sum that’s $1 million more than what Forty Seven raised when it spun out of Stanford in 2016. At that time, scientists had a good understanding that targeting 47 had applications in blood cancers, Barkal said. One of the goals of her research in the Weissman lab was to find ways to apply the same approach to solid tumors. For solid tumors, blocking 47 led to a lot more variability in getting macrophages to recognize cancers, Barkal said. That variability suggested cancer cells are using another shield—a different don’t eat me signal.
The title of Barkal’s Ph.D. dissertation is “Boosting macrophage appetites for cancer immunotherapy.” What scientists know now that they did not know at Forty Seven’s origin is that there are multiple don’t eat me signals present in tumors, Barkal said. She was the lead author of a paper published in Nature in 2019 that explained this research. The greatest expression of CD24 was observed in ovarian cancer cells, according to the paper. Scientists also found that this protein was abundant in triple negative breast cancer cells. Blocking 24 on both breast and ovarian cancer cells led to increased macrophage eating.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Share some of the trends you are seeing among your clients across healthcare, including chronic conditions, behavioral health, healthcare navigation, and more.
There is a reason Barkal did not name her company “Twenty Four.” While the 24 protein is highly expressed in breast and ovarian cancers, it might have a mixed role in other tumor types. In some cases, the appropriate therapy might involve blocking both 47 and 24. In yet other types, the best approach might be to go after an altogether different cancer protein. To leverage these signals in immunotherapy, the key is to understand which of the signals are present in any given tumor. Pheast’s technology is a platform that sorts through the don’t eat me signals in order to find the dominant one (or two). It’s not necessary to block all the don’t eat me signals, Barkal said. Blocking the dominant or co-dominant signals should be enough to whet the appetites of macrophages.
“The goal is to remove the don’t eat me input to tip the balance toward eating. We don’t need to cover 100%,” of don’t eat me signals, she said. “We need to cover the majority.”
Future combinations could include pairings with other types of cancer drugs, potentially including a different blockade therapy called a checkpoint inhibitor, a class of drugs that encompasses Merck’s Keytruda and Opdivo from Bristol Myers Squibb. These drugs block checkpoint proteins that keep T cells from recognizing tumors. Ovarian and triple negative breast cancers have historically had weaker responses to T cell immunotherapies, Barkal said. That suggests an additional approach, such as enlisting macrophages, could offer a way to better address these tougher-to-treat tumors.
Forty Seven’s CD47-blocking drugs are antibodies. Antibodies were used in the 24-targeting research that was published in Nature but Barkal said Pheast’s therapies could come in a range of modalities. However, one of the problems with the antibody drugs that target 47 is that this protein is also found on red blood cells, which means that blocking it also makes it recognizable to macrophages. In the Nature paper, the scientists wrote that a 24-blocking antibody showed no detectable binding to red blood cells. But the paper also notes a different potential off-target effect. CD24 is abundant on B cells, so targeting the protein with a drug could deplete these immune cells.
Pheast bears the imprint of its forebearers. The startup’s current team of fewer than 20 includes veterans of either Forty Seven or Weissman’s lab. Barkal said that her company’s expansion includes a search for her successor. Currently interim CEO, Barkal said she plans to remain involved with Pheast as principal founder. Investors in Pheast’s Series A financing include Catalio Capital Management, Arch Venture Partners, Alexandria Real Estate Equities, Risk and Reward, and the Stanford University Presidential Venture Fund. Barkal said Pheast’s goal is to bring CD24-targeting therapies into clinical trials, though she declined to offer a timeline. She added that the financing will enable the startup to broaden the scope of its technology beyond CD24.
“That’s really the long-term vision,” Barkal said. “Go after don’t eat me signals more globally in cancer.”
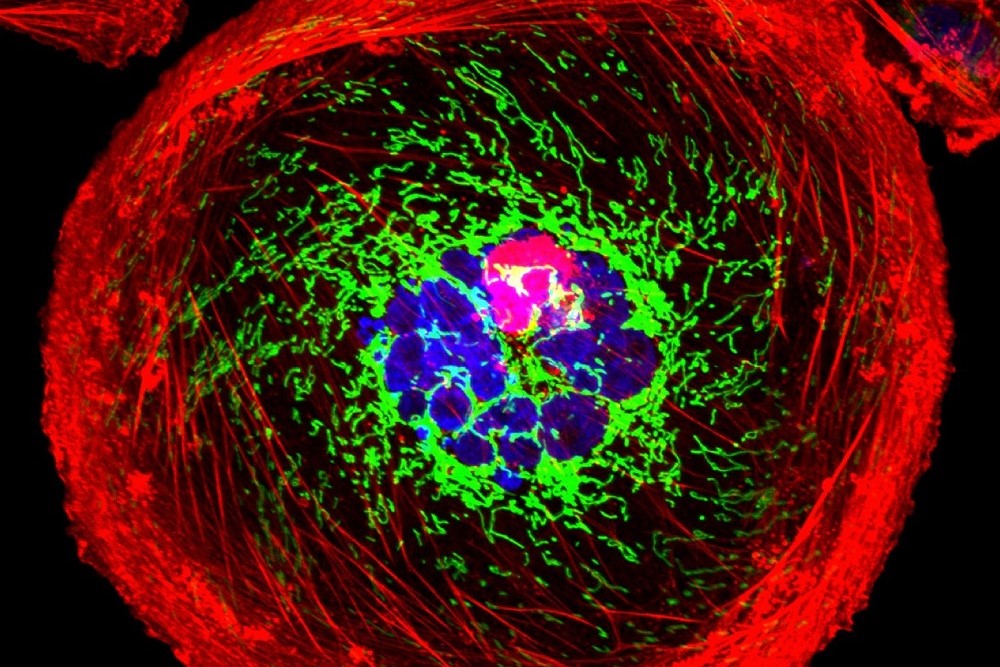
Public domain image by the National Cancer Institute














