Creating a family is one of the most natural progressions in life, essentially preserving our collective future since the beginning of time. Family structures are fashioned in unique configurations but the desire to care for, nurture, and love one’s child is universal. The extraordinary elements that must perfectly collide to create life is nothing short of miraculous, yet pregnancy is so often taken for granted, underrated as commonplace. That is, until one is faced with the understanding that the “common” flow of life does not apply to them.
Whether the inhibiting factor is infertility, biology, or a matter of circumstance, the hopelessness of a lost dream is excruciating. Understanding the delicate factors involved, IVF practitioners aspire to be the source of encouragement to prospective parents in the face of this overwhelming challenge.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Iris Har-Vardi Prof. Iris Har-Vardi, Ph.D., serves as the Director of Fertility and IVF Lab at Soroka University Medical Center. She is also a Senior Lecturer at Ben Gurion University in the Faculty of Health Sciences. Prof. Har Vardi established and serves as a lecturer of the National Fertility Course for embryologists for licensing under […]
The current state of IVF outcomes
Since the first IVF baby was born in 1978 the field of embryology and in vitro fertilization (IVF) have transformed the impossible into possible for prospective parents who suffered from infertility. However, possible does not mean simple, and the statistics for IVF success haven’t seen much movement over the last few decades. In fact, only 30-40% of women will realize a live birth in the first round of IVF. One such cycle can cost between $12k-$25k, making this a risky business with no guarantee of a positive outcome.
A major driver of this statistical stagnation is the lack of standardization of practice in the field. Patients receive varied treatments leading to high differentiation in outcomes. Though embryologists are extremely well educated and highly skilled, success rates for embryo selection are inconsistent at best. Lacking a consistent system for collecting and interpreting end-to-end data on this process, IVF is ripe for disruption.
Embryology practice determines the successful formation of life

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
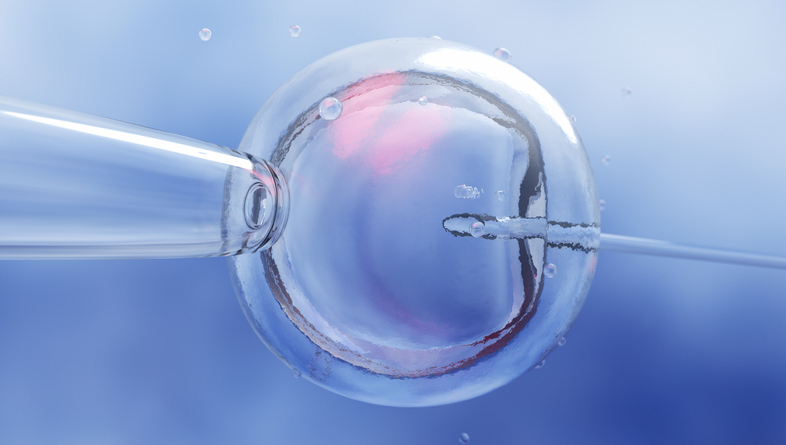
IVF is dependent on the field of embryology. Embryologists trained in the study of formation, growth and development of an embryo, and are tasked with assessing which embryo to choose for transfer in hopes of resulting in a live birth.
Typically, embryologists place a fertilized egg in an incubator and manually check the progress under a microscope over a five-to-six-day period. The discretion is up to the embryologist on how many times per day they assess and make notes of development, typically looking on day one, day two or three, and on day five to assess if the embryo is viable.
The process of carefully removing a developing embryo from an incubator to observe under a microscope and notate the data is time-consuming. The highly technical task of safely maintaining the beginnings of life outside of the body leaves little room for error. Embryologists assess a developing embryo using approximately five data points available to human analysis. Even with their extensive training, education and clinical experience, so few developmental milestones in embryo development leave much room for variation in decision making.
IVF professionals rely on their education, basic assessment parameters and their own experience to make decisions. For perspective, imagine getting blood work results with no established parameters that indicate a range of normal limits. Diagnosis and any treatments would be based on the discretion of the observer and not on any evidence-based standards. This analogy explains the frustrating status IVF has operated in, until now.
Empowering embryologists with AI-driven decision support
When assessed under a microscope, an embryologist may look once a day at several morphologic characteristics of an embryo to determine its viability. However, with the introduction of time-lapse monitoring systems to the IVF lab, there is an opportunity to leverage new computer vision and AI technology that can capture images at almost any developmental stage of an embryo and assess additional developmental details that are not obtainable by the human eye. An AI system trained by ‘experienced eyes,’ captures and processes a large database of embryos developing in time-lapse incubators, analyzing these data combined with treatment outcomes. Based on this the AI provides information to help embryologists make consistent, data-driven decisions. This in turn should result in more consistent decision-making among embryologists and lead to improved pregnancy and live birth results.
AI bridges the gap of human error and maximizes the potential success rates of IVF. AI’s ability to analyze big data paves the way for improving IVF outcomes and the development of evidence-based parameters that establish a consistent standard of care.
Financial implications of embryo selection accuracy
The ability to improve consistency in viable embryo selection also affects the financial investment and minimizes patient risk with fewer cycles to live birth. A cycle of IVF is the process of ovarian egg retrieval, fertilization, observing and selecting a viable embryo for transfer, and finally transferring the embryo in hopes of implantation. Two weeks later the patient will get the first pregnancy test result. This three-week process is an emotional journey, an expensive journey, and one with frustratingly low odds of success.
Additionally, IVF is not without risk to patient health due to the procedure of egg retrieval, and multiple embryo transfer to increase chances for viable pregnancy and cost mitigation. With AI-assisted consistency in embryo selection, you can diminish unnecessary cycles and risks. The decision support tool IVF clinicians have in AI analyzed data supports transparent, explainable, evidenced-based information that invites prospective parents to the decision-making table.
A bright and hopeful future awaits the 90 million couples globally struggling with infertility. AI that provides explainable, transparent data that IVF clinicians can understand and trust, is poised to advance IVF success rates that have stagnated for too long. Infusing transparency through this process will transform the daunting unknown into a hopeful process. Children are our greatest commodity and most cherished gift. With AI assistive technology, the natural flow of life can be available to everyone.
Prof. Iris Har-Vardi, Ph.D., serves as the Director of Fertility and IVF Lab at Soroka University Medical Center. She is also a Senior Lecturer at Ben Gurion University in the Faculty of Health Sciences. Prof. Har Vardi established and serves as a lecturer of the National Fertility Course for embryologists for licensing under the Israeli Health Ministry and Controller of Standards of IVF Units for the Israeli Health Ministry. She lends her extensive experience to Fairtility, where she serves as Scientific Director, as the company transforms IVF treatments through its transparent AI decision support tool, CHLOE EQ. She holds a Ph.D. from Ben Gurion University in microbiology and immunology.












