Historically, healthcare has been primarily focused on treating the symptoms of disease. Outside infectious diseases, whether that was preventing the acid indigestion with H2 blockers and PPI or using or anti-inflammatories to reduce pain and swelling in patients with arthritis, or reduce elevated blood pressure with beta blockers and calcium channel blockers, we developed palliative treatments based on a mid-20th century understanding of how the human body works.
The 21st century brought a very different understanding of disease based on an unraveling of the precise molecular and genomic underpinnings of disease. We are now at a crossroads where we can envision a future in which we no longer simply palliate the symptoms of chronic disease, we outright cure it. In regard to cancer specifically, we are no longer limited in attempting to selectively poison cancer cells like bacterial invaders, rather we target therapy to address the flaws in the molecular and genetic blueprint that gave rise to the cancer cells and the immune cells that are blind to them.
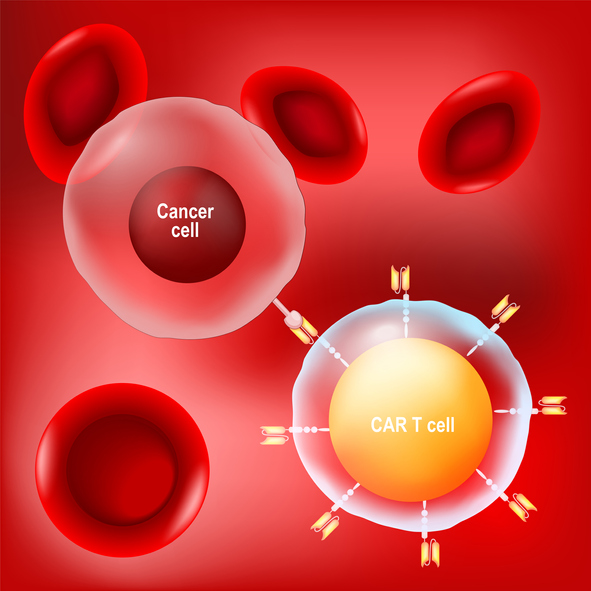
One of the most prevalent examples of therapies derived from this way of thinking are CAR-T treatments, which have changed the face of healthcare.
Five years of CAR-T
This specialized treatment that modifies a patient’s T-cells to treat rare blood cancers was approved by the FDA just five years ago. The lengthy process involves collecting T-cells from patients (autologous), modifying T-cells to produce proteins called chimeric antigen receptors (CARs) on their surface, and infusing the modified cells back into the patients — enabling the cells to find and kill cancer cells.
CAR-T has become increasingly recognized as an exciting and potentially paradigm-shifting treatment in the past five years. In fact, more than 10,000 patients have undergone this new treatment for certain types of leukemia, lymphoma and multiple myeloma.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Bruce A. Feinberg Dr. Bruce A. Feinberg is the Vice President and Chief Medical Officer at Cardinal Health Specialty Solutions. He is nationally recognized for his expertise in specialty oncology and the business of specialty healthcare. He has been instrumental in the development of clinical pathways in oncology care —which aim to control costs, improve […]
As more patients receive CAR-T, we continue to gain real-world data about how this treatment works long-term. One exciting result is that by using a patient’s own body to fight the disease, the human body not only fights in the moment, but stores the memory of how to fight reoccurrences years down the road. To further solidify this evidence, several patients involved in the very first CAR-T clinical trials have been declared cancer-free for more than a decade.
While this treatment is not without its own safety concerns, oncologists and patients are increasingly adopting it, while clinical trials are proving it is both safe and effective in earlier lines of treatment. With a success rate of about 30% to 40% for durable remission, CAR-T treatments are the only FDA-approved therapy to show significant benefit for those patients who, as few as five years ago, had no other treatment option. This success rate led to the FDA approving the treatment earlier in a patient’s cancer care journey, and many oncologists believe that CAR-T will eventually become a first-line treatment.
But, before we reach that point, we need to account for several logistical hurdles specific to these treatments.
Overcoming logistical and access hurdles
While cost is an often-cited concern about these treatments, researchers are finding that the evidence for efficacy is outweighing the high price tag for some oncologists. The problem may not be the cost/benefit ratio but a coverage system that is not designed for curative treatment, the value of which might be amortized over decades.
Beyond the sticker price, oncologists often cite the administrative burdens of using these therapies, such as cumbersome logistics and long referral processes and payer approvals. These obstacles can often result in these fragile patients not being able to receive the treatment at all. Such delays and burdens are complicated by the limited number of centers approved for CAR-T administration. Due to the serious and potentially life-threatening side effects that patients can experience following the infusion of the modified T-cells, only around 200 centers across the country have received the accreditation and training to deliver the treatment.
These obstacles are not insurmountable, however. In the past five years we have seen progress in addressing each, resulting in the medical communities’ increasing interest in — and adoption of — CAR-T.
The future of medicine from a CAR-T lens
As we improve these processes for a treatment that has potential to impact much more than a handful of hematologic cancers, medical science has not slowed its progress. Other methods of manipulating the immune system to recognize and destroy cancer are currently being explored. One such treatment is moving CAR-T from autologous – using the patient’s own cells — to allogeneic — an off-the-shelf option that can be used by many patients (similar to universal blood donors). This would drastically reduce the logistical and administrative burden, as well as cost of therapy, while still producing similar benefits.
Other efforts have been built on the monoclonal antibody-based therapies developed in the early phase of biologic drugs. Modifying the antibodies such that they are bi-specific, allows them to simultaneously bind to both cancer cell and immune cell, literally overcoming the absent immune recognition of cancer by bringing the immune cells directly to the cancer cells.
CAR-T is just a piece of this future of medicine. In the short term, our biggest opportunity is in cancer treatment. We know that empowering the host instead of killing cancer cells with toxins is more effective. There is a huge array of cancer opportunities, and it all begins with one question: can we identify a target that is somewhat unique to that cancer cell that can begin the process of targeting? Then, we can translate that into a genetic modification of a T-cell so that it gets to the target.
This new world of mediated cancer-based therapies is wide open. The number of clinical trials underway gives me hope and makes me believe that within the next five years, we’ll have many more breakthroughs.
Dr. Bruce A. Feinberg is the Vice President and Chief Medical Officer at Cardinal Health Specialty Solutions. He is nationally recognized for his expertise in specialty oncology and the business of specialty healthcare.
He has been instrumental in the development of clinical pathways in oncology care —which aim to control costs, improve the quality and increase predictability—key factors in developing a sustainable approach for caring for patients with high-cost diseases. A highly sought-after speaker on cancer-related topics who regularly publishes in peer-reviewed journals, he is also the author of the bestselling Breast Cancer Answers and its follow-up book, Colon Cancer Answers.














