Eisai now has the most detailed look yet at the clinical trial data for its Alzheimer’s disease drug lecanemab, with results showing reductions in telltale disease indicators and a slowing of clinical decline. But the results come amid recent reports of two patient deaths in the study, raising questions about whether the benefits from the drug outweigh renewed concerns about its safety risks.
The Japanese drugmaker, which is developing lecanemab under a partnership with Biogen, presented the full trial data on Tuesday during the Clinical Trials on Alzheimer’s Disease (CTAD) conference in San Francisco. When the companies released preliminary results in September, they reported that treatment with the drug led to a statistically significant 27% reduction in clinical decline measured at 18 months. Data presented at CTAD and published simultaneously in the New England Journal of Medicine provided additional context.
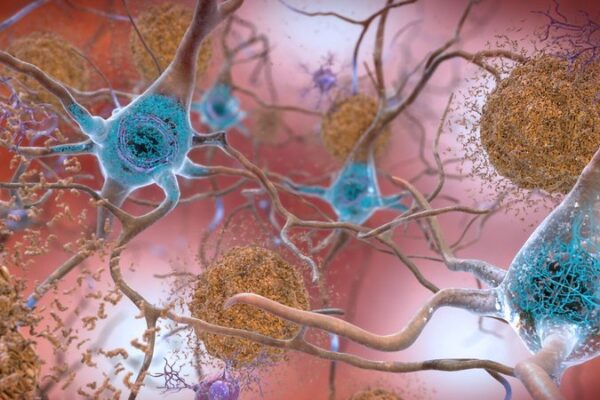
Lecanemab is a monoclonal antibody designed to bind to protofibrils of amyloid, aggregates of this toxic protein that are thought to play a role in Alzheimer’s disease. The placebo-controlled Phase 3 study testing the drug enrolled 1,795 patients with early-stage Alzheimer’s. The study included those who have other conditions, such as hypertension, diabetes, heart disease, and obesity. Study participants were permitted to continue taking medications to manage those conditions.
Patients were evaluated according to Clinical Dementia Rating Sum of Boxes (CRR-SB), which quantifies the severity of dementia symptoms in several areas according to a rating scale that runs from 0 to 18. Results reported at CTAD showed that the average change in score from baseline at 18 months was 1.21 for the lecanemab group and 1.66 for the placebo group. The 0.45 point difference is enough to be statistically significant. It’s also enough to be clinically meaningful for patients, said Sharon Cohen, medical director and site principal investigator at Toronto Memory Program. Most Alzheimer’s experts feel slowing of the disease by 20% to 30% is meaningful for patients. For patients, what matters is still being able to drive, to work, to cook dinner. What does not matter to them is a score on a cognitive test, she said. But that difference in score does translate into a difference in the patient’s quality of life.
“It’s not one number, it’s a group of numbers that tell us yes, patients are benefiting in multiple ways,” Cohen said, speaking during a Tuesday night briefing with journalists. “Yes it matters, patients tell us it matters.”
Chrisopher Van Dyk, director of the Alzheimer’s Disease Research Unit at the Yale School of Medicine, called the 27% reduction in clinical decline a starting point. Starting treatment even earlier, in patients who are pre-symptomatic, may lead to even better results, he explained. The results also open the door to potential combination studies. The 27% benefit from lecanemab could be supplemented by treatment with different drug or drugs that work in different ways. Drug combinations is an approach advocated by the Alzheimer’s Drug Discovery Foundation.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Share some of the trends you are seeing among your clients across healthcare, including chronic conditions, behavioral health, healthcare navigation, and more.
Data analysis also suggests that the slowing in clinical decline continues to improve over time. Trial data were extrapolated to 30 months. At 25.5 months, the difference in scores was 0.68. Cohen said that this result suggests cumulative benefit—the longer a patient is on the drug, the greater the benefit extends beyond the 27% observed at 18 months. In a research note, William Blair analyst wrote that while more studies are needed to confirm this result, the projection shows the potential benefit from continued treatment with the drug.
There is a lot that requires further study to better understand the effects of lecanemab. One perplexing observation was the loss of brain volume, a change that is typically associated with neurodegeneration, Van Dyck said. While overall brain volume decreased, that change was not observed in the hippocampus, a region of the brain that plays a role in learning and memory. Van Dyck said the loss of volume could be related to fluid shifts due to treatment with the drug, but he added the reason remains unclear.
Despite the benefit observed with lecanemab treatment, the recently reported patient deaths make safety concerns top of mind. One death in October was reported by Stat. This week, the journal Science reported details of a second death. In both cases, patients were taking blood thinners concurrent with receiving lecanemab. Both deaths were attributed to severe bleeding in the brain, a known adverse event risk of the Eisai drug.
William Blair analyst Myles Minter said in a Wednesday research note that the fatalities suggest a small but increased risk of serious bleeding when patients treated with lecanemab are also taking anticoagulants. In the Phase 3 study, 4.5% of patients enrolled take such drugs. But that risk could be higher. Minter added that recent studies suggest real world use of anticoagulants reaches as high as 20% of Alzheimer’s patients.
Both deaths occurred in the open-label extension study, where anticoagulant use is permitted with informed consent about the risk of cerebral hemorrhage. In its announcement of the trial results, Eisai steered the blame away from its drug.
“Both cases had significant comorbidities and risk factors including anticoagulation contributing to macrohemorrhage or death,” the company said. “Therefore, it is Eisai’s assessment that the deaths cannot be attributed to lecanemab.”
Lecanemab is expected to receive an FDA decision by Jan. 6. That decision is under an application submitted for accelerated approval based on results from a Phase 2 study. The results reported at CTAD are from a Phase 3 test that the FDA has agreed could serve as the confirmatory study supporting an application seeking full regulatory approval.
Eisai Chairman and CEO Ivan Cheung said during the media briefing that his company has been fully transparent with patients about the data surrounding lecanemab. All safety data will be shared with regulatory agencies and the company will discuss with them the best way to share those data with prescribers and patients. As for whether the bleeding risk warrants a strict warning on the drug’s label, Cheung said it’s too early to say. That discussion will happen if the company receives an affirmative accelerated approval decision, he said. But Cohen said that information about these risks will need to be provided to clinicians.
“Some people may need closer monitoring,” Cohen said. “If someone is at higher risk of side effects, you monitor them more closely. Education will have to roll out to prescribers on how to deal with this issue.”
If lecanemab receives accelerated FDA approval, Cheung said Eisai plans to submit an application for full approval “within days.” That application will be followed by regulatory filings in Europe and Japan.
Asked whether the FDA might convene a meeting of an independent advisory committee, a move typically made when the agency wants additional input on questions about a drug’s safety, Cheung said Eisai has not received any indication that regulators want such a meeting for lecanemab. He added that he can’t yet say whether the FDA will want an advisory committee meeting to discuss potential full approval of the drug. That communication cannot happen until the after the company files its application.
Public domain image by Flicker user NIH Image Gallery














