
The classic battle between time and the best interest of the patient is real in primary care.
The average primary care doctor has between 1200 to 1900 patients, with Kaiser Permanente reporting a mean per-physical panel size of 1,751. This most likely is not accurate nowadays, with some reports saying 2500 to 4000 is the new norm, as stated brilliantly by a LinkedIn comment by Sharon Ng M.D.
I asked my followers to share their thoughts on how they can make the healthcare system better, and they posted some great comments on this Linkedin Thread – 70 comments and counting.
What does this mean?
Basically, primary care doctors do not have much time to do anything but the basics and very little time for preventive care measures.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Jonathan Govette Website Jonathan Govette is the Co-Founder at Oatmeal Health, an AI-enabled teleradiology and patient engagement service that coordinates lung cancer screenings for underserved, vulnerable patients. Oatmeal Health is a veteran-owned and clinician-led platform changing how self-insured employers, FQHCs, and payers manage population risk and improve outcomes. Through its discovery of novel AI systems, […]
With basic math you can see the numbers do not add up, 24 hours in a day, proper care takes 26.7 hours. And unfortunately, we are not robots that can work non-stop or manipulate time with the Infinity Gauntlet or have special powers like Dr. Strange to make up the difference.
PCPs were estimated to require 26.7 h/day, comprising
- 14.1 h/day for preventive care
- 7.2 h/day for chronic disease care
- 2.2 h/day for acute care
- 3.2 h/day for documentation and inbox management
“There is this sort of disconnect between the care we’ve been trained to give and the constraints of a clinic workday,” said Dr. Justin Porter, assistant professor of Medicine at the University of Chicago and lead author of the paper. “We have an ever-increasing set of guidelines, but clinic slots have not increased proportionately.”
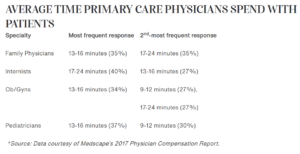
With most doctors spending less than 15 to 20 minutes with their patients per visit, there is not much time for fact-finding, let alone education for the doctor to learn what preventive screening resources are available for their patients, even if that care is reimbursable by Medicare/Medicaid, such as a lung cancer screening.
To many chronic disease screenings to manage
Chronic diseases are a leading cause of morbidity and mortality worldwide, and preventative screenings are the most effective way to reduce the risk of developing a chronic disease. However, many individuals do not take advantage of preventative screening services for chronic diseases, especially in rural areas.
Another study from Duke in 2005 calculated that doctors would need an additional 10.6 hours per workday to manage the top 10 chronic diseases among their patients.
And it has real consequences for the delivery of health care; the researchers said that time pressure helps explain why improvements in outcomes have not kept pace with advances made in the field, the study said.
If you do surveys with patients about what frustrates them about their medical care, you’ll frequently hear, ‘My doctor doesn’t spend time with me’ or ‘My doctor doesn’t follow up,’” said Porter in the UChicago article. “I think a lot of times this is interpreted as a lack of empathy or a lack of willingness to care for a patient. But the reality—for the majority of doctors—is simply a lack of time.
Why is this?
The bottom line is the education of the physician, time, and patient access. All things can be fixed if given the proper allocation of resources and expertise.
With 59% of all Americans (194 million) suffering from at least one chronic disease, and almost one in three adults having three or more chronic conditions doctors are tasked with doing the impossible. ent lives and cost of care for risk-bearers.

Source: Rand Corporation
The authors suggested “team-based care,” where nurses, physician assistants, counselors, and others help to deliver recommended care, as one solution to the problem of overworked, burned-out primary care docs.
Using team-based care, they estimated that the amount of primary care physician time could decrease to 9.3 hours per day.
Photo: malerapaso, Getty Images
Jonathan Govette is the Co-Founder at Oatmeal Health, an AI-enabled teleradiology and patient engagement service that coordinates lung cancer screenings for underserved, vulnerable patients.
Oatmeal Health is a veteran-owned and clinician-led platform changing how self-insured employers, FQHCs, and payers manage population risk and improve outcomes.
Through its discovery of novel AI systems, the company is enabling the full potential of its platform to identify high-risk patients early and intervene with screenings before their health worsens so healthcare costs don't spiral out of control while delivering a better experience to families, employers, clinicians, and health plans.
Jonathan received his B.S. from California Polytechnic University in San Luis Obispo, He developed optimal referral pathways and created the first-of-its-kind referral management platform in 2010. Jonathan was selected as the winner of Samsung's Digital Health Conference, a finalist in Venturebat's Health Beat Conference, and a Techstars / Cedar Sinai Alumni.
Trusted healthcare technology expert quoted in Forbes Magazine, HIMSS, Medcity News, Beckers Healthcare, Newsweek, Techcrunch, Modern Healthcare, and others. Collaborations with Cleveland Clinic, Harvard Medical, and AARP.














