
2025 has been declared the year of the AI agent. While that may be true in general, it’s not accurate in healthcare. In our industry, 2025 is undoubtedly the year of the scribe.
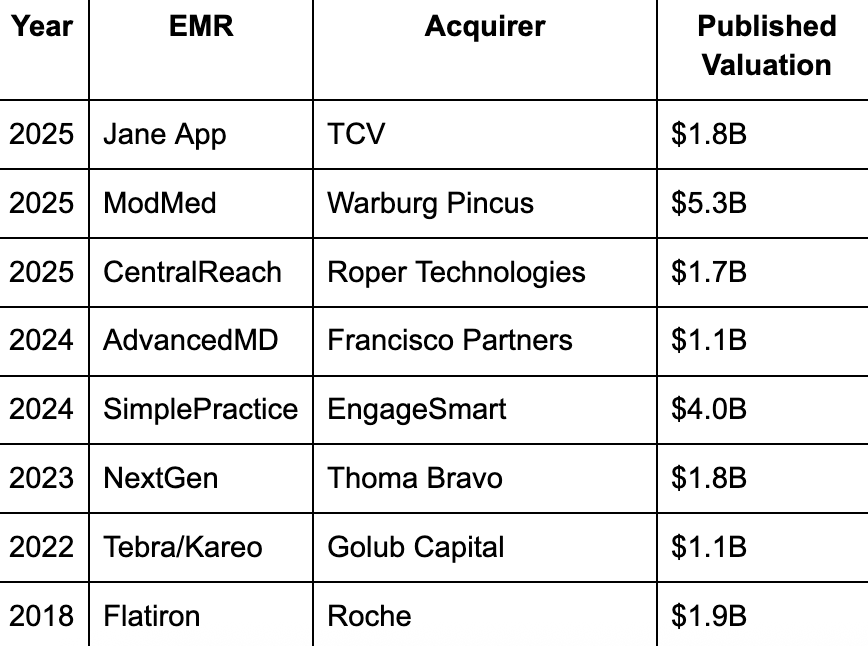
Abridge, Ambience and other ambient AI scribes have attracted unprecedented venture capital interest and valuations this year. Meanwhile, established electronic medical record (EMR) companies with large and sticky customer bases, like the ones below, are passing around private equity owners at multiples of around 10x revenue or less.

The Power of One: Redefining Healthcare with an AI-Driven Unified Platform
In a landscape where complexity has long been the norm, the power of one lies not just in unification, but in intelligence and automation.
With this, we must pause and reflect on the state of the EMR landscape and what it means for an AI-enabled future in healthcare. Each of the health tech businesses above has built a significant clinical, financial and operational user base in a trillion-dollar total addressable market, but has not hit anywhere near the multiples investors are paying for scribe companies today.
Why? Traditional EMRs aren’t designed for it. They’re built for compliance and billing capture, and use outdated paradigms in architecture and user experience design. They can’t build breakout software businesses, let alone platforms that can live in the future where AI agents become integrated parts of the care team. Instead of creating new opportunities, traditional EMRs are constraining AI’s potential in healthcare.
The future of healthcare is agentic
We are rapidly approaching a future that goes well beyond the scribe. One that integrates AI across the full spectrum of clinical, financial and operational jobs within an outpatient practice. In this world, specialized agents work within a unified data architecture and chain together with multiple other agents across the patient journey.
For example, a scheduling agent automates self-serve patient booking and triggers the intake agent to bring informatics into the chart, which in turn provides deeper context for the documentation agent and/or clinical copilot supporting the clinician during the visit. Post-visit activities are connected and automated to code, scrub, suggest documentation gaps and manage the revenue cycle.
All of these use cases are coming fast and threaten the lifespan of traditional EMRs that don’t adapt to the pressure.
It must be integrated
There are a few challenges the new agentic world presents to the incumbent:
- One is the user experience; how do we design so that the human decision maker is in control?
- Another is safety; how do we protect against hallucinations and bugs, and continuously evaluate to refine prompts and improve the system?
- A third is data integration and platform capabilities; an agent is only as good as its tools and context.
There are more questions when we get into technical and architectural detail.
- Where should each agent be hosted?
- How will shared context be maintained across agents without creating dangerous inconsistencies?
- When one agent makes a change that affects other agents’ work, how will that coordination happen in real-time?
Without proper orchestration, each new agent means additional brittle integration points and potential conflicts, creating a compounding, exponential coordination challenge.
One way around this is to build agents into the EMR, with a suite of bundled AI products across jobs like smart intake, chart summary, ambient scribe, and coding automation. For EMR companies with the architecture and technical capabilities to accomplish this, they can offer AI tools where users already are, augmenting their core experience and avoiding orchestration challenges since agents leverage a common underlying system and data model.
Nothing matters without evals
What’s missing from all of the hype posts and videos on social media are tangible results. The industry needs to prioritize transparency into the effectiveness of AI tooling and establish benchmarks that validate its safety. We must move beyond launch announcements and prototypes into the world of continuous evaluation of the safety of AI tools, testing them against expert clinical judgment.
Mainstream adoption for agents and AI in healthcare won’t be reached without evaluation rubrics and continuous feedback loops between human practitioners and agentic solutions to continuously improve models and ensure we are safely augmenting clinical decisions. The human clinician and agent must co-exist, and agents must have the tools and context to drive their own improvement.
It won’t be possible with traditional EMRs
The legacy market doesn’t have APIs, software developer kits or data access that AI solutions can use to integrate into existing workflows or evaluate their safety. Without this, our option is a tab in the browser and a copy/paste manual workflow or a lowest common denominator interface that allows data to move across systems and users, but does not allow for coordination. This blocks autonomy; agents can’t work together in the existing paradigm.
Systems like the ones in the table above and other names not listed, like athenahealth, eClinicalWorks, and AllScripts, which have dominated outpatient care, have not been built for this new future. Their strategies and resourcing indicate that they will maximize the current SaaS paradigm and move slowly (if at all) to support the new one. That has a great cost for clinicians and patients.
As an industry, we have a duty to adopt AI and to test it to the edge of its capabilities. But we must do this with awareness of the high stakes of healthcare automation, constantly keeping the safety of patients top of mind. Our opportunity is to do this work well, and urgently, and reach the transformative potential of AI in healthcare.
Editor’s note: Neither the author nor his company have any relationship with the companies/products mentioned.
Photo: ipopba, Getty Images
Adam Farren is the CEO of Canvas Medical, the EMR platform accelerating everyday medicine. Prior to Canvas, he was CGO at Elation Health and Osmind, and led growth strategy and go-to-market across venture-backed startups in financial services, education technology, and media. Adam holds a bachelor’s degree from Princeton University and an MBA from the Haas Business School at the University of California, Berkeley.
This post appears through the MedCity Influencers program. Anyone can publish their perspective on business and innovation in healthcare on MedCity News through MedCity Influencers. Click here to find out how.









