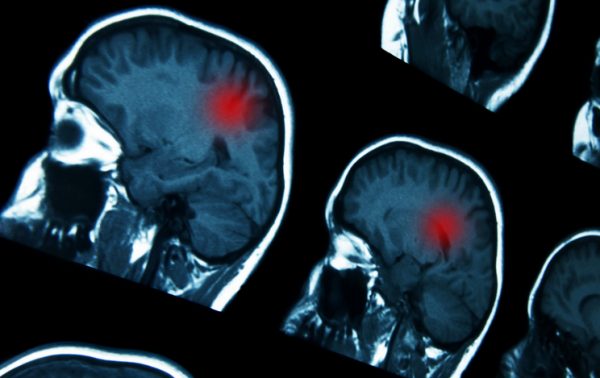
A study conducted by Bristol-Myers Squibb combining its immunotherapy agent with radiation in patients with the most aggressive form of brain cancer has failed, the drugmaker said.
New York-based BMS said Thursday that its Phase III CheckMate-498 study of PD-1 checkpoint inhibitor Opdivo (nivolumab) plus radiation in patients with newly diagnosed MGMT-unmethylated glioblastoma multiforme, or GBM, failed to meet its primary endpoint of improving overall survival.

Behavioral Health, Interoperability and eConsent: Meeting the Demands of CMS Final Rule Compliance
In a webinar on April 16 at 1pm ET, Aneesh Chopra will moderate a discussion with executives from DocuSign, Velatura, and behavioral health providers on eConsent, health information exchange and compliance with the CMS Final Rule on interoperability.
Shares of BMS were down 1.1 percent in Thursday morning trading on the New York Stock Exchange.
Another Phase III study, CheckMate-548, evaluates Opdivo in combination with radiation and the drug temozolomide in MGMT-methylated GBM patients. MGMT methylation is known to confer a somewhat better prognosis. CheckMate-548 is expected to reach primary completion in February 2022.
Temozolomide received Food and Drug Administration approval in 1999 and, having since gone generic, is the last FDA-approved drug established to improve overall survival in GBM, along with Novocure’s Optune device. To date, however, GBM remains an incurable and invariably fatal cancer, with a median survival from diagnosis of less than two years.
First-line treatment consists of surgical resection, temozolomide and radiation, but it inevitably relapses, after which treatment options are limited. Roche’s drug Avastin (bevacizumab) received full FDA approval to treat recurrent GBM in December 2017, having previously received accelerated approval based on data indicating it improved progression-free survival – the amount of time patients live without their cancer growing – but not overall survival. However, even the study that led to Avastin’s full approval in GBM still did not show a significant increase in overall survival. The drug works by targeting tumor vasculature, which in turn starves tumors of the blood they need to grow.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
BMS announced the failure of a Phase III trial of Opdivo in recurrent GBM, CheckMate-143, in August 2017. The ClinicalTrials.gov database does not currently list any Phase III studies of other PD-1 or PD-L1 checkpoint inhibitors in GBM. Opdivo’s nearest competitor, Merck & Co.’s Keytruda (pembrolizumab), is in several academic-led Phase II studies for the cancer.
Although the field is littered with numerous failures, several companies have sought to develop new therapies for GBM.
These include San Diego-based Tocagen, which is developing a therapy that involves a combination of a retroviral replicating vector-based therapy called Toca 511 (vocimagene amiretrorepvec), which delivers an enzyme derived from yeast into cancer cells. Patients are then injected with Toca FC, a formulation of the inactive prodrug 5-fluorocytosine, which in cancer cells infected with Toca 511 is converted into 5-FU, an anti-cancer agent used in many chemotherapy drugs. The combination therapy is currently in a Phase III clinical trial.
Photo: goglik83, Getty Images












