
Most consumers are satisfied with their health insurance plans, but are looking for better communication on their coverage and costs. That’s according to a study released Thursday by HealthEdge, a Burlington, Massachusetts-based software provider for health insurance companies.
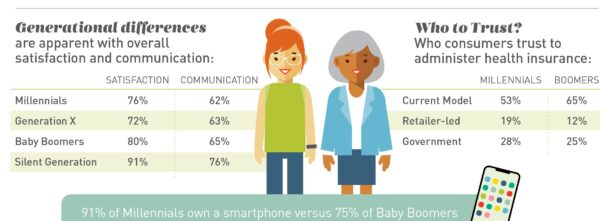
HealthEdge surveyed more than 5,000 people online for the study, which focused on primary holders of health insurance. According to the results, 78 percent of the respondents were satisfied with their overall health plan, while just 65 percent were satisfied with communication from their current insurer.

Behavioral Health, Interoperability and eConsent: Meeting the Demands of CMS Final Rule Compliance
In a webinar on April 16 at 1pm ET, Aneesh Chopra will moderate a discussion with executives from DocuSign, Velatura, and behavioral health providers on eConsent, health information exchange and compliance with the CMS Final Rule on interoperability.
The factors that weighed most negatively on these scores mainly fell under costs and understanding coverage. The biggest negative impacts for respondents’ satisfaction with their insurance plans included knowing if a treatment would be covered, the affordability of their coverage, and understanding out-of-pocket costs.
“I don’t think it’s unusual to say that health insurance is one of the last industries where it’s not easy for a consumer to get that kind of (cost) information,” said Harry Merkin, vice president of marketing for HealthEdge. “People want to know, “if I go to an urgent care facility, what’s it going to cost me? If I go to a MinuteClinic, what’s it going to cost?”
Interestingly, the survey showed a shift in attitudes about health insurance between generations. The vast majority of respondents from the silent generation were satisfied with their overall insurance, at 91 percent. Gen X respondents, on the other hand, were the least satisfied at 72 percent, with millennials only marginally happier with their plans.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
But all generations agreed on a few points: They would be more satisfied with plans if they offered more tools to understand their benefits and compare costs, as well as incentives for healthy behaviors.
In the three years that HealthEdge has conducted the survey, Merkin said this year he noticed a marked interest in health incentives across the board.
“Across all generational groups, everybody is willing to accept incentives for healthy behaviors. That is relatively new. It’s never been as pronounced across all of the different age groups as it was this time,” he said. “The population of the U.S. is saying, ‘We’d like to be healthier and we’d like you to help us do it.’”
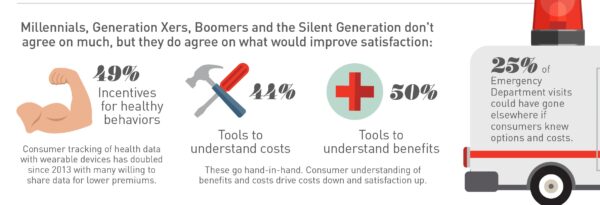
For example, that could include offering a discount for gym memberships, or for users that reach a certain number of steps using wearable devices. These types of benefits can help companies attract workers and save on health care costs in the long-term, Merkin said.
“If you can use proactive incentives to help prevent a heart attack or diabetic shock, the savings are going to be enormous,” he said.
From a communication perspective, insurers can improve in a few big ways, he said. For example, health plans still lag behind in adopting member portals. And even when that information is available, many beneficiaries still don’t access them.
Payers and providers can also partner with community resources to ensure patients have access to food, transportation, and other critical ingredients for their health.
“The elusive part of this has been linking up with community resources. For example, someone being able to take meditation or some sort of community exercise class at the YMCA,” Merkin said. “Where it’s working, it’s a partnership on the ground between the resources closest to the community and closest to the population.”
Brand intelligence research company Survata conducted the survey on behalf of HealthEdge. Between Aug. 29 and Sept. 7, 2019, 5,137 people who were the primary holder of health insurance were surveyed online. Respondents were distributed across age groups and U.S. regions, and the majority of respondents were female, at 76 percent.
Photo Credit: Minerva Studio, Getty Images












