
An aerial view of downtown Alamosa in the spring. The city in southwestern Colorado has seen seven Covid-19 cases.
In southwestern Colorado, San Luis Valley Health quickly made preparations for a potential surge in Covid-19 cases. The health system, which has a 49-bed hospital and a 17-bed critical access hospital, added inpatient and ICU beds. It turned one of its outpatient clinics into a respiratory clinic with ventilators.
Colorado saw an early influx of Covid-19 cases, reporting 8,286 cases as of Friday, according to data from Johns Hopkins University. Many of them are concentrated near the state’s ski resorts and major metros, but less populous counties have reported cases, too.

With the Rise of AI, What IP Disputes in Healthcare Are Likely to Emerge?
Munck Wilson Mandala Partner Greg Howison shared his perspective on some of the legal ramifications around AI, IP, connected devices and the data they generate, in response to emailed questions.
Nestled between the Great Sand Dunes and the toothy San Juan Mountains, the five-county area making up the San Luis Valley has seen 23 cases and two deaths attributed to Covid-19. As of Thursday, San Luis Valley Health had treated six to eight Covid-19 positive cases, CEO Konnie Martin said.
“We’ve certainly had Covid and had some sick patients with Covid, but it hasn’t created that kind of rush to healthcare services that we’ve seen in other parts of the country,” she said. “It’s a relief, it’s what you hope for.”
The converse of that, Martin said, has been detrimental. Since cancelling elective procedures in mid-March, the hospital has been seeing 30% to 40% as much traffic as it would normally get this time of year. The emergency room had less than half as many cases as it did in March.
“Our business has just plummeted. We’ve stopped elective procedures and well visits. We’ve brought to a halt so many of the services that we provided,” she said. “Over the last few weeks, the financial impact has been difficult. … It has proven to be as much of a challenge as managing Covid itself.”
Like many of its peers, San Luis Valley Health has shifted some workers down to part time, and furloughed some employees. Martin said the hospital was looking into every avenue of support it could find, from federal funding to donations. The hospital has received donations from private foundations and stimulus funds allocated through the CARES Act, but more is still needed.
“One of the most important things is we’ve got to chart a path forward. We have to have a healthcare system for our communities — in particular, our rural communities,” she said.
San Luis Valley Health has a level 3 trauma center, it offers surgery, has an oncology center, and delivers the community’s babies. The nearest hospital with comparable services is 120 miles away.
The 10,000-person city of Alamosa, which houses a university and a regional airport, needs those services.
“We’re critical for this community,” Martin said.
Cases across the U.S.
In every community, the picture is a little bit different. Some, like Alamosa, have had relatively few cases. Others have seen a surge in cases, such as the ski towns of Vail, Colorado and Sun Valley, Idaho.
Numerous meat-packing plants have also reported clusters of Covid-19. Near Hazleton, Pennsylvania, a Cargill meat processing plant announced last week it would temporarily close, after 130 of its 900 workers tested positive for the virus, according to the Philadelphia Inquirer. Tyson Foods closed a plant in Columbus Junction, Iowa, with 86 cases tied to the plant, according to the Quad City Times.
Three-quarters of rural counties have reported at least one case.
“It’s there. It’s just a question of how bad it’s already there,” National Rural Health Association (NRHA) CEO Alan Morgan said in a phone interview.
There are roughly 2,000 rural hospitals across the U.S. More than half of them are critical access hospitals, meaning they have 25 or fewer inpatient beds, offer 24-7 emergency services, and are generally a long distance from any other hospital.
On average, these hospitals might have one or two ventilators, if any at all, Morgan said. If there are relatively few critically ill patients, that’s fine. But in areas where there are large clusters of Covid-19, such as near New Orleans, patients get transferred to larger facilities.
“They were able to transfer but transfer times got excessively longer, because New Orleans got swamped,” Morgan said.
The good news, Morgan said, is that most of these hospitals have taken the necessary steps to prepare for the pandemic, including triage services and making dedicated capacity for Covid-19 patients. The bad news is that process is costly, and many of these hospitals are already strapped for cash.
Funding problems magnified
One chilling estimate by Guidehouse showed that a quarter of rural hospitals are at a high risk of closing. The vast majority of those hospitals are considered essential to their communities. Prior to the pandemic, these hospitals already faced razor-thin margins and a decline in utilization.
Eight hospitals have already closed this year, and two in the middle of the pandemic. In West Virginia, 141-bed hospital Fairmont Regional Medical Center closed its doors on March 19. Its owner, Alecto Helathcare, had previously said it would close the hospital, but shuttered it a month earlier than expected. In Tennessee, 40-bed Decatur County General Hospital closed on April 15, leaving 21 counties without a hospital.
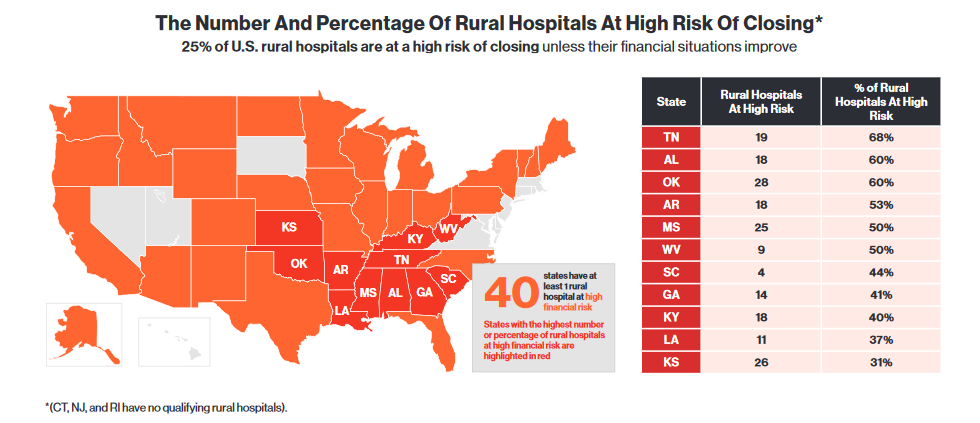
States with the most rural hospitals at high risk of closing, from Guidehouse’s 2020 Rural Hospital Sustainability Index.
David Mosley, a partner with Guidehouse and the former director of finance for North Carolina’s Medicaid program, described some of the issues factoring into the crisis. A shift in jobs to metro areas means most patients in smaller communities are covered through Medicaid, Medicare, or have no insurance at all. In many of these cities, hospitals are the largest employer.
On top of that, many hospitals in rural communities have seen a decline in the number of patients. Sometimes, this is because the cities themselves have gotten smaller. Other times, patients forego care in their community to drive to a larger facility in the closest metro, even for lower acuity procedures.
“There are many cases where people are driving by their local hospital for the care they’re receiving, when it’s just as good or better,” Mosley said.
Add a month’s worth of cancelled surgeries on top of that, and the financial burden multiplies. Roughly 70% to 80% of rural hospitals’ revenue comes from outpatient services or elective surgeries.
“Any decrease in incoming revenue is crushing,” he added.
Right now, hospitals have an average of 30 days’ cash on hand, NRHA’s Morgan said. Thankfully, they’ve gotten a little bit of funding to tide them over for the next month. Of the $100 billion set aside for healthcare providers under the CARES Act, the first $30 billion was allocated based on Medicare spending, which would help many hospitals in these communities.
“It was specifically targeted toward rural communities which was wonderful,” Morgan said.
Come mid-May, these hospitals will have burned through most of that funding. In a letter to the Department of Health and Human Services, the American Hospital Association said the next wave of funding should target hospitals in Covid-19 hotspots, hospitals with lots of Medicaid and Medicare Advantage patients, and rural hospitals.
Hospitals have also been able to receive advance Medicare payments, which would allow them to get payments for the projected costs they would bill. That helps too, Morgan said, but this mechanism effectively works like a loan.
For her part, Martin said San Luis Valley Health had received some funding through the CARES Act, but had too many employees to qualify for the Payroll Protection Act. She said the hospital was looking into all of its options for financial support, and trying to plan for what the coming months will hold.
“We’re trying to do all the research we can on what is available through the federal packages and potentially some state support,” she said. “We’re looking at how to restart our business; how to get ready for what the new normal is going to look like for a bit. It’s really just uncharted grounds.”
Photo credit: Jacob Boomsma, Getty Images














