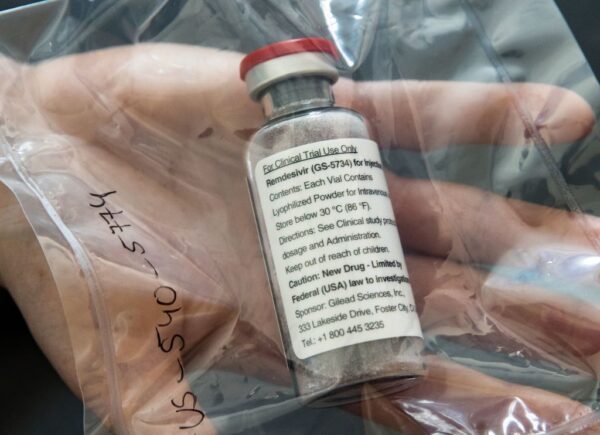
The jury is still out on whether Gilead Sciences’ investigational drug against Covid-19 is effective, but while the first fully enrolled, double-blind study could have data out in a couple of weeks, authorities in Japan aren’t waiting, according to news reports.
Reuters reported Friday that the National Institute of Allergy and Infectious Disease’s Phase III trial of Foster City, California-based Gilead’s remdesivir was running ahead of schedule and could have results out by the middle of next month, citing an interview with the study’s principal investigator. Meanwhile, Japanese news service Kyodo News on Monday reported that Prime Minister Shinzo Abe said authorities there would soon approve remdesivir for Covid-19, with another government official adding that it could happen as early as May. The Kyodo report noted that after Gilead files for approval in Japan, regulators will fast-track the approval, and that the streamlined approval is available under the condition that the drug has been approved in another country.

Behavioral Health, Interoperability and eConsent: Meeting the Demands of CMS Final Rule Compliance
In a webinar on April 16 at 1pm ET, Aneesh Chopra will moderate a discussion with executives from DocuSign, Velatura, and behavioral health providers on eConsent, health information exchange and compliance with the CMS Final Rule on interoperability.
In a note to investors Monday, RBC Capital Markets analyst Brian Abrahams wrote that the report from Japan came despite “equivocal” data so far on remdesivir. He noted that results of the Gilead-sponsored clinical trial in patients with severe disease are expected by the end of the month, but that the study is unlikely to produce definitive answers due to its lack of a control arm. Meanwhile, more definitive data are expected from Gilead’s study in patients with moderate disease, whose results are expected in late May, as well as the aforementioned NIAID-sponsored study.
The equivocal data in question come from a slow drip of results from various studies, including a few dozen patients receiving remdesivir under compassionate use protocols, a leaked description of results from a single center in Gilead’s clinical trials and prematurely released data from a terminated Chinese study.
The compassionate use data, on 53 patients, lacked a control arm, but indicated that patients with severe disease were benefiting from the drug. The same is true of results from a single center – the University of Chicago – that were discussed in a leaked video regarding 125 patients, mostly in the severe-disease trial. However, data from a double-blind, placebo-controlled study among severe-disease patients in China, briefly posted on the World Health Organization’s website, indicated the drug did not produce a benefit, but the sample lacked sufficient statistical power for any firm conclusions. That trial had been terminated early due to lack of available patients for enrollment.
Abrahams wrote that, per communication with Gilead, the Chinese study data’s hazard ratio of 1.23 for time to benefit for the drug versus placebo indicated that patients on the drug trended to a 23% better time to improvement. However, he wrote that many key questions still remain, such as the rationale for clinical benefit in more severe patients.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
Photo: Ulrich Perrey, Pool/AFP, Getty Images












