
Where should learning begin on how to create a five-star patient experience?
- In mid-career, mandated empathy-training sessions?
- After a physician has received low survey ratings for poor bedside manner?
- After a particularly bad experience with a patient
- Or, as one advances in their career, considering that emotional (vs. cognitive) empathy increases with age.
Those are all times when physicians can begin to learn about the attitude and behavior required to deliver better patient experiences. Yet, none is quite right; we believe medical school is the optimal time to develop a holistic, grounded understanding of how to improve the patient experience. Why? Because one’s views on the culture— the way people and institutions do things—of medical practice are formed in medical school. In this article, we look at one school that does a particularly good job in the development of bright med students into empathetic caregivers.
Brody School of Medicine
East Carolina University’s Brody School of Medicine works particularly hard at ensuring its students develop compassion. Of the 155 medical schools in the US, Brody doesn’t crack the US News & World Report top 50. As national reputation determines 40% of the final ranking score, top schools in the report include large, well-funded, and obvious places like Johns Hopkins, Harvard, Stanford and Columbia. If judged by inventions, medical advances, and recognition, these highly respected medical schools likely produce the smartest, most technically adept physicians.
To retain their overall best ratings, the schools need to be great in areas including student MCAT scores, academic achievement of their students, awards and prizes granted to school and graduates alike, research excellence, grant funding, teaching excellence, and traditionally recognized metrics across numerous medical specialties (i.e. cardiology and neurology). Further, they need to communicate their multi-variate excellence, accept into their ranks candidates who may help extend reputational excellence in these areas, and evaluate and graduate students based on achievement in these areas.

Health Benefit Consultants, Share Your Expert Insights in Our Survey
Joe Mandato and Ryan Van Wert MD Joe Mandato has spent his career leading numerous high-growth organizations developing disruptive technologies used in clinical healthcare settings. He has often held overall responsibility for his teams’ strategic implementation of programs designed to enhance and improve the clinician-patient experience. Today, he invests in and serves on the boards […]
The possible drawback of the broad, sweeping excellence of these schools is that they may not be able to focus—truly focus, with their strategy, time, attention and money—on teaching students how to deliver a very caring, effective interaction with a patient. If a medical school is going to help drive enduring changes to improve the patient experience, it needs to focus on advancing that change across multiple areas, mainly:
- In its communications to the world so that it attracts the applicants it wants
- In the application and admissions process
- In its curriculum, and
- In the assessments and evaluations of students.
Delivering an outstanding, compassionate patient experience needs to be a driving and prioritized feature of medical education. This is where Brody comes in. It appears to do this more consistently and comprehensively than other medical schools. It has chosen to clearly position itself in the family- and primary-care physician segment. It consistently is ranked as the number one or two medical school in the country at producing family physicians by The American Academy of Family Physicians. And it’s ranked in the top ten percent in the country in the combination of primary care and serving rural or under-served populations.
We examined the Brody way of excelling in each of the four areas highlighted above—Communications, Admissions, Curriculum, and Evaluations—as relates to focusing on a superior patient experience.
Communications & Marketing
Brody knows its mission and sticks to it. It communicates clearly and consistently that it is the right medical school for North Carolina residents who want to focus on the compassionate delivery of general practitioner medicine within and among rural and under-served populations (and research programs that target chronic diseases relevant to these populations). Here’s a sample of communications, showing it knows what it is:
The Brody School of Medicine at East Carolina University is nationally recognized for preparing primary care physicians who practice in medically underserved communities. All those admitted are North Carolina residents and the majority of its graduates practice primary care in North Carolina. Brody’s research includes a strong focus on cardiovascular disease, diabetes and preventive care
and
The school consistently ranks in the top 10 percent of U.S. medical schools for graduating physicians who practice in-state, practice primary care and practice in rural and underserved areas.
Admissions
When it comes to applicants, Brody seeks and evaluates applicants on their capabilities in family medicine. One article quotes the president of the American Academy of Family Physicians as saying, “Brody is the quintessential example of how you recruit these young people to the specialty of family medicine.”
One way it does this is to cost substantially less than most other schools—especially considering its requirement that applicants be NC residents (i.e., they get in-state tuition). It is able to draw applicants who might otherwise think the high cost of medical school makes it a non-option for them. At Brody, only 13% of students have medical debt over $200K compared to 37% nationally, and Brody students graduate with an average of 26% less debt than their peers nationwide. This low debt increases the likelihood they’ll choose primary care, despite the lower pay compared to other specialties. (Data from AAMC 2020 Graduation Questionnaire.)
The school says its low costs allow graduates to choose specialties based on their hearts, not their pocketbooks. And isn’t that where the idea of “love” in medicine starts? Choosing a specialty you love, not that you think will pay best? The comparatively low costs may also partly explain how Brody’s 2020 entering class composition is 53% non-Caucasian (compared to, for instance, 24% at Harvard) and how 25% of students are over age 25 as compared to 16% nationally. It’s terrific that those who are older and realizing that they want to serve humankind through medical nurturing and caretaking may choose to enter the field.
The school vets candidates based on the totality of their experiences, references, interviews and character. It states, “. . . we strive to use numerical data (such as GPAs and MCAT scores) more as a ‘safety gauge’ than as an absolute measure of worthiness.” Indeed, the aforementioned character elements show up more often and more prominently in school communications than do items like MCAT scores and grades. Compared to much larger schools, the language that Brody uses is more compassionate, relatable, and human. Our quick scans of communications by schools considered elite schools more often use somewhat technical, achievement-based words and phrases like:
excellence, accomplishment, talents, instructions, policies, deadlines, essays, academics, MCAT, powerful, science, technologies, excel, research, committee, competence.
Meanwhile, Brody more often, in its communications about the types of students it admits, makes use of relationship-based, compassion-oriented words and phrases like:
rich, rewarding, collegial, relationships, take time, call us, improve, prepare, know all of their classmates, journey, shared experience, counseling, patient care, teaching, curiosity, enjoy, experience, success, enriching.
It’s logical to infer that they attract and evaluate their med school candidates based on candidates’ composite ability to be part of those words—a rich, rewarding, collegial experience.
Medical schools such as Harvard, Yale and Johns Hopkins do not use only bureaucratic, technical language when speaking to and attracting applicants. Those schools certainly use words like support, diversity, culture, and patients in their admissions literature. And it’s not as if Brody, for its part, is one big hug-and-relationship-festival in its apparent assessment of applicants, because it also uses more technical and/or bureaucratic terms like challenging, commitment, science, administration, foundation, standards, and achievements. The difference in the language of admissions is not dramatic, but it is clear in showing that Brody tries especially hard to attract and admit students who are committed to a career of compassionate care.
We reached out to Brody, and here’s what we learned from Dr. Cedric Bright, associate dean for admission. He said, “The admissions process at Brody focuses on objective and subjective measures. Objective measures such as MCAT, GPA and hours of clinical and community activities are reviewed as the foundation of the application. Subjective components round out the applicant and include eight personal characteristics or attributes that we must have in our students, such as communication, empathy and values diversity.” He continued, “Our interview process includes an Emotional Intelligence interview and situation-based judgment questions to assess the emotional maturity of our applicants and to further confirm the presence of the aforementioned personal characteristics in our potential students.”
Curriculum
As far as the Brody curriculum, one of the first things that strikes us is the apparent culture of the classroom. One student said in an article, “Here there really is no pride [as in, excessive ego]. I was amazed by how little pride there was and there are these awesome doctors who really focus on the mission to serve the community.”
The curriculum is geared towards delivering a strong patient experience as a form of medical excellence. It includes a course in the foundational years called “Society, Culture, and Health Systems.” The school redesigned its curriculum to promote principles [emphasis added by us]:
- To better prepare graduates to work in tomorrow’s health systems by incorporating health system science training in all phases. (n.b.: this is the “understanding of social and systemic forces in health systems)
- To integrate basic, clinical, and health systems science to improve health and care delivery
- To focus on promoting, supporting, and maintaining health, not just treating disease
- To promote the development of leadership skills, professionalism, ethics, humanism and service to others
It also focuses on “professional identity formation, wellness, lifelong learning skills and reflection.” Early on, forming one’s identity as—in addition to a very smart, hard-charging scientifically minded person—also a caretaker of others who, at an especially vulnerable time, may be disabled, depressed, worried, confused, etc., is important.
Another core competency that Brody students must develop in order to advance through the four years of medical school is interpersonal and communication skills. This means they must “demonstrate effective listening, verbal and written communication skills that result in the effective exchange of information and collaboration with patients and families while providing patient centered care.” (If you’ve read our articles, you’ll know that in our own experiences, doctor-patient communication and collaboration haven’t always been the case). More specifically, Brody students will:
- Communicate compassionately and effectively…
- Develop therapeutic relationships with patients and their families across a broad range of cultural and socioeconomic backgrounds…
- Engage in shared decision making with patients and heathcare colleagues as evidence by listening, providing them with anticipatory guidance, and negotiating with empathy and respect for autonomy and lifestyle choices.
- Collaborate and communicate effectively … in a manner that maintains a climate of respect, collegiality, and adaptability focused on patient and population centered care.
Assessments & Evaluations
As far as assessments and evaluations for advancement based on a patient-centered skillset, Brody professors conduct evaluations of students’ performance in clinical courses by answering 21 questions about their observed behaviors. These areas are considered to be behavioral anchors that allow professors to observe progress in developing a patient-centered skillset. Here’s an example—it reads from a less skilled mark (left side) to a more skilled grade (right side):
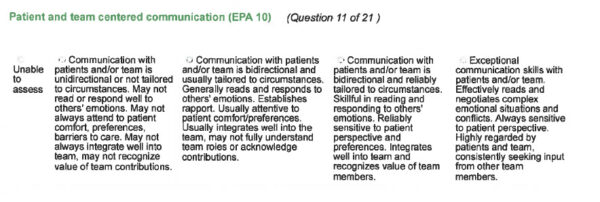
Source: Brody School of Medicine
It’s a Wrap
Brody aligns its communications, admissions, curriculum, and assessments with the idea of patient centeredness. In our view, the school has the right stuff for helping med students develop compassionate caretaking skills. It consistently prioritizes patient-centered care and communication and a holistic and longitudinal relationship with patients. The Brody model is worthy of emulation nationally, but its mission is decidedly local—to increase the supply of primary care physicians serving the state, to improve the health status of eastern North Carolina’s citizens and to enhance access of minority and disadvantaged students to a medical education.
Brody is one great example of medical schools that you may not know about but that are doing a very fine job training our next generation of patient-centered, compassionate caretakers in medicine. As you well know, we don’t pretend to comprehensively evaluate medical education, and we haven’t done a deep or broad statistical analysis here. Further, we deeply admire the large, research-based medical schools where students and professors advance the standard of care for all patients nationally and globally; they are foundational to excellence in medicine. Still, Brody reaches into our hearts, shows us that there’s another side to medicine to complement other extraordinary schools. Brody ought to be considered equally as extraordinary . . . a healthcare institution that’s playing a key part in improving health and aging in America.
It’s been shown patients can benefit from a satisfying medical experience as well as from the actual clinical treatment. The satisfying medical experience, even in the presence of average and not extraordinary medical treatment, leads to trust, follow-through, health improvements, and more. We suspect Brody graduates learn more than do many medical school graduates about providing that satisfying medical experience for all patients.
Now if only those patient-centric graduates could practice in a health sector where insurance pays for them to spend time really getting to know patients. (We wrote about insurance in this article.)
Joe Mandato has spent his career leading numerous high-growth organizations developing disruptive technologies used in clinical healthcare settings. He has often held overall responsibility for his teams’ strategic implementation of programs designed to enhance and improve the clinician-patient experience. Today, he invests in and serves on the boards of companies in the life sciences. He also writes about and teaches the business of healthcare.
Ryan Van Wert, MD has worked as an intensivist in critical care settings, where he gained deep understanding of the realities of the physician-patient interface. He has led medical device and IT companies, including his current role as co-founder and CEO of Vynca Health, which specializes in enabling improved advanced care directives among patients and providers. In these roles, Ryan has learned a lot about patient engagement and healthcare communication. He is also assistant director at the Stanford Byers Center for Biodesign.













