An Imara drug that hits a novel target to treat rare, inherited hemoglobin disorders has failed two mid-stage studies, one for sickle cell disease and the other for beta thalassemia. The biotech company said Tuesday it will discontinue both programs.
In preliminary results, Imara said its drug, tovinontrine, failed to distance itself from a placebo in either clinical trial. The small molecule is also being developed as a potential treatment for a type of heart failure. In light of the disappointing data from the blood disorder studies, Boston-based Imara said it is weighing its options for that program, as well IMR-261, a drug candidate that offers an alternative approach to treating hemoglobin disorders.
“Moving forward, we plan to consider our strategic options, including development of tovinontrine in heart failure with preserved ejection fraction (HFpEF) as well IMR-261 clinical development plans,” Imara President and CEO Rahul Ballal said in a prepared statement.
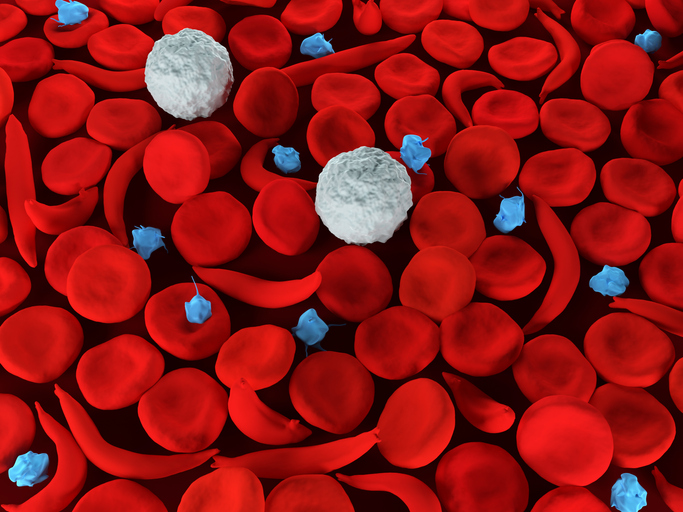
Tovinontrine is a small molecule designed to target and block an enzyme called phosphodiesterase-9 (PDE9). This enzyme selectively degrades a signaling molecule that plays a role in vascular biology. By blocking PDE9, the Imara drug is intended to boost the levels of this key signaling molecule. Tovinontrine was hoped to lead to higher levels of fetal hemoglobin that reduces the sickling of red blood cells characteristic of sickle cell disease. This approach was also tested in beta thalassemia, a disorder that leads to lower hemoglobin levels.
The main goal of the Phase 2b sickle cell study was to measure annualized rates of vaso-occlusive crisis, which is when the sickle-shaped red blood cells block blood flow and deprive tissues of oxygen. According to the preliminary results released Tuesday the reductions in the rates of these crises in patients treated with tovinontrine were not enough to be statistically significant compared to the placebo group.

A Deep-dive Into Specialty Pharma
A specialty drug is a class of prescription medications used to treat complex, chronic or rare medical conditions. Although this classification was originally intended to define the treatment of rare, also termed “orphan” diseases, affecting fewer than 200,000 people in the US, more recently, specialty drugs have emerged as the cornerstone of treatment for chronic and complex diseases such as cancer, autoimmune conditions, diabetes, hepatitis C, and HIV/AIDS.
In beta thalassemia, the main study goal was to assess the drug’s safety and tolerability in patients who are transfusion dependent as well as those who are not dependent on transfusions to treat their disease. For those who depend on transfusions, the study also evaluated the drug’s ability to reduce the transfusion burden. In both the low and high doses of tovinontrine tested in the beta thalassemia study, Imara reported “no meaningful benefit was observed in transfusion burden.”
If there’s a bright spot for tovinontrine, it’s that the drug was well tolerated by patients, showing no safety problems that could stand in the way of tests in other indications. In January, the FDA cleared Imara’s application to begin human testing of tovinontrine in heart failure with preserved ejection fraction. Last month, in its report of fourth quarter and full year financial results for 2021, Imara said it expected to dose the first patient in a Phase 2 study in the heart failure indication in the second quarter of this year.
Imara still has another opportunity to address hemoglobin disorders. Last October, the company acquired from Complexa a compound named CXA-10, which the Berwyn, Pennsylvania-based biotech had tested in the rare kidney disorder focal segmental glomerulosclerosis and pulmonary arterial hypertension. The small molecule, now renamed IMR-261, is designed to activate a transcription factor called Nrf2. Imara has said this approach that has the potential to increase fetal hemoglobin, and could offer a way to treat hemoglobin disorders and iron disorders.
Image: Meletios Verras, Getty Images














