
President Trump Can Act Now To Make Healthcare Affordable
The Trump administration can immediately take these two price transparency administrative actions to reduce costs and improve affordability.

The Trump administration can immediately take these two price transparency administrative actions to reduce costs and improve affordability.
Despite all the noise around the updates, there’s one area that’s been conspicuously absent this year: enforcement of patient estimate requirements.

Alan Murray on improving access for medical transportation.

Inaccuracies don’t just erode trust — they lead directly to surprise billing events, missed appointments, care delays, and in some cases, enforcement action.
CMS recently announced that it will change the administrative fee that providers and insurers must pay when initiating a reimbursement dispute under the No Surprises Act — the agency is lowering the fee from $350 to $50. This move came a week after the Texas Medical Association won a court case challenging HHS over its 600% price hike on the fee.

Amid the difficult healthcare environment, it's important to note that there have been some wins for employers, said Katy Spangler, senior advisor of the American Benefits Council, during the Midwest Business Group on Health conference held Tuesday. These wins include the No Surprises Act and price transparency rules.
Patricia Kelmar, healthcare campaigns director at the Public Interest Research Group, is an advocate for the No Surprises Act. But there's one thing that bothers her: the fact that providers can ask patients to waive their surprise billing protections, she said Tuesday when speaking at the AHIP Medicare, Medicaid, Duals and Commercial Markets Forum in Washington, D.C.

In a landscape where complexity has long been the norm, the power of one lies not just in unification, but in intelligence and automation.
If the NSA-implementing agencies could plot out and publish their plan for adopting standards, publishing regulations, and setting new compliance dates for the NSA AEOB and provider directory requirements, it would help tremendously to level set on expectations and help organizations budget and plan for actual implementation.

Implementing and pursuing innovation in digital health and healthcare IT should be a priority for all U.S. healthcare providers and payers — especially as the lessons and response to the Covid-19 pandemic become permanently part of our everyday lives.

Although the “Requirements Related to Surprise Billing: Final Rule,” was released on August 19th, the No Surprises Act roll-out is far from complete. Its complexity means adherence, oversight, and enforcement, as well as system and process changes, are still works in progress.
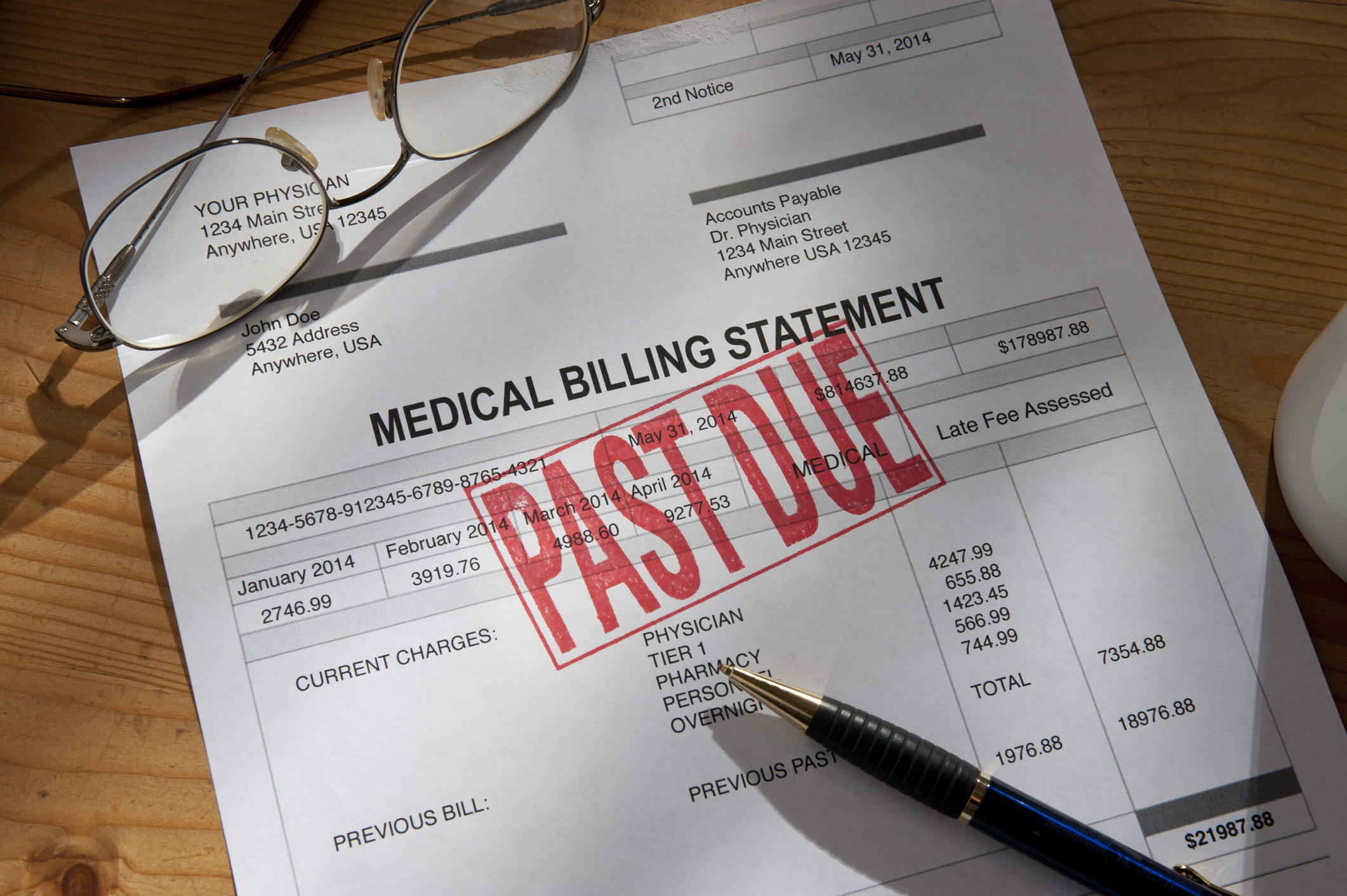
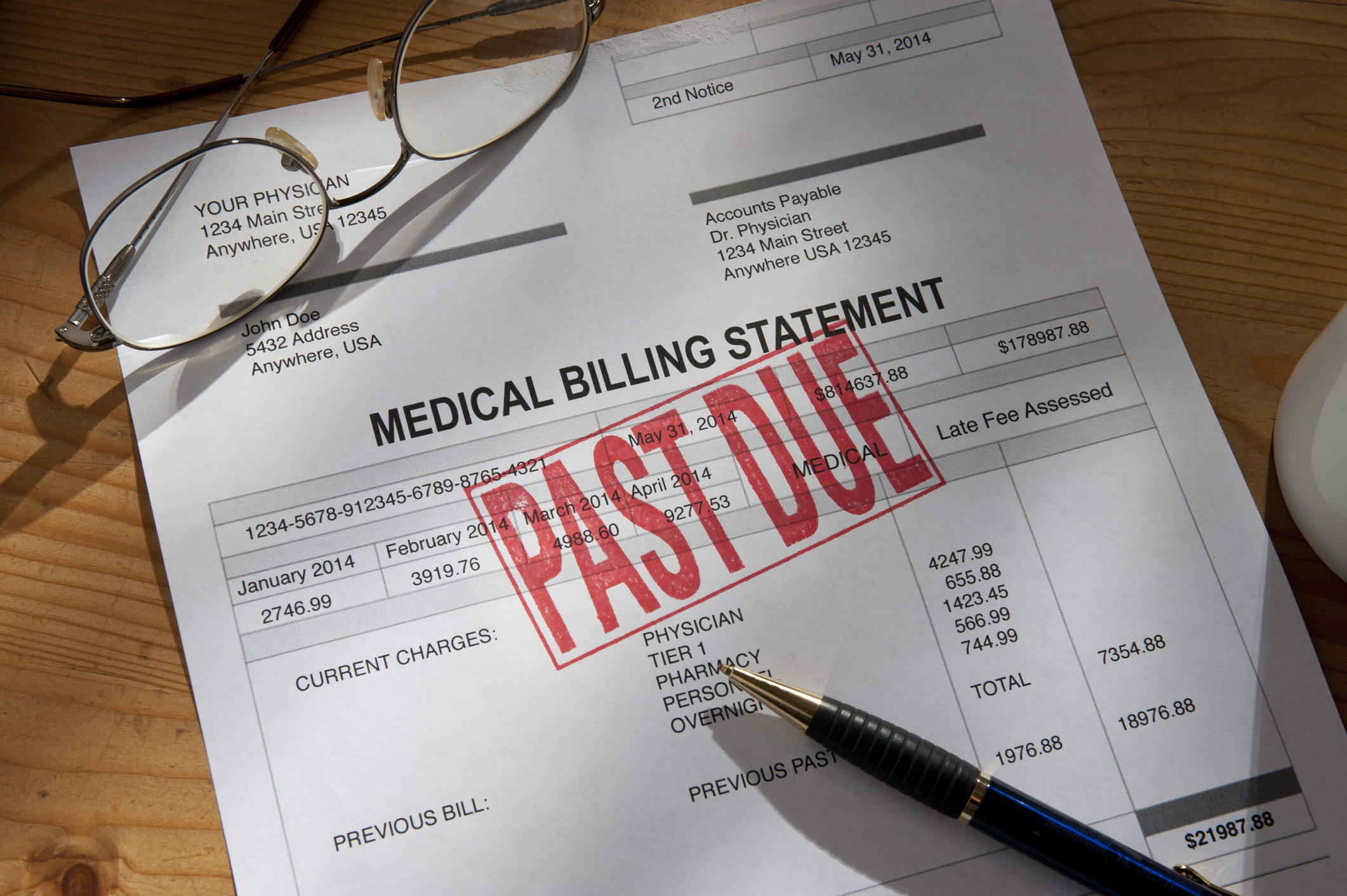
Skyrocketing medical bills and a lack of understanding in the healthcare system is putting financial stress on Americans in 2022, several recent reports have found. Despite the No Surprises Act, which protects consumers from surprise billing, many Americans said they’re still receiving unexpected bills, and a low healthcare literacy is making it difficult for them to know how to handle high medical bills, the surveys find.
Patients deserve high-quality care and better outcomes, as well as equitable, consistent and transparent billing experiences. So how do we get there?

This legislation has the potential to drastically reshape the economics of healthcare in America, but it remains unfamiliar to those it affects most—namely, patients, doctors and outpatient surgery centers.

Therapists say their professional codes of ethics already require disclosure to patients of per-visit costs. Requiring diagnostic billing codes in the estimate before even seeing a patient — as they interpret the rule — is unethical, they argue, and tallying up what might be weeks or even months of treatment costs could keep some patients from undergoing care.

Betty Chow, a Los Angeles resident, had a cervical disc replaced in August 2020 at a surgery center that was part of her Anthem Blue Cross PPO network. Thirteen months later, she was blindsided by a bill for nearly $2,000 from the anesthesiologist who was on her surgical team but was not contracted with her […]

The Texas Medical Association (TMA) filed a brief on Monday to further oppose the ruling on the No Suprises Act that currently allows aribtrators to use the average in-network rate to determine out-of-network cost.